CHILBLAINS
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it

Chilblains are a vasospastic inflammatory disorder that occurs several hours after of the skin of unprotected individuals has been exposed to a non-freezing cold in damp environment (temperate humid climates).
Chilblains are less common in countries where the cold is more extreme because the air is drier and people have specially designed living conditions and clothing.
They are sometimes aggravated by sun exposure.
Chilblains are diagnosed on clinical grounds: they appear as single or multiple (usually symmetric) small, tender, itchy, erythematous-to-violaceous/purple swollen, indurated patches, papules or plaques on a cool, edematous base.
They affect the body's exposed extremities, such as backs and sides of the toes and fingers, the face (nose, cheeks, earlobes) legs (heels, shins, thighs, and hips), wrists of babies. In severe cases lesions can progress to blistering or ulceration.
The color in people with dark skin shows marked darkening
Chilblains usually develop several hours after exposure to the cold in temperate humid climates. They are usually accompanied by intense burning, itching or pain, which can become more intense going into a warm room.



After riding a motorcycle in the rain with air temperature near the 0 C° or young, horse-riding women are also somewhat more susceptible! This group of women ride their horses for hours during winter months (kibes). Their tight and improperly-insulated riding outfits squeeze skin and blood vessels and, thus, interfere with the intricate cold temperature response mechanism leading to large, tender chilblains-like spots with a lumpy consistency on the lateral calves and thighs.
Horse-riding enthusiasts who wear tight clothing in cold weather may develop similar lesions on the thighs.
They occur when a predisposed individual is exposed to cold temperasture and humidity. The condition is also known as pernio or perniosis: it is a localised form of vasculitis (the cold damage tiny blood vessels – capillaries - in the skin).
Chilblains do not appear immediately but appear a short while after being in the cold.
Chilblains are not painful at first, and they rarely cause any permanent damage and will normally heal within a few weeks if further exposure to the cold is avoided.


Chilblains can occur at any age, but are more common in children and the elderly. The condition also affects women more than men. People with poor circulation, are more susceptible to the condition. In children recurrences each winter for a few years are common but complete recovery is usual. Chilblains in elderly people have a tendency to get worse every year unless precipitating factors are avoided.
Arterial circulation is normal on physical examination.
Signs and Symptoms of chilblains

A sign is something the doctor detect while a symptom is something the patient feels and reports. For example, pain may be a symptom while a rash may be a sign.
Chilblains should be suspected in people with one or more intensely itchy, painful, swollen skin lesions that appear within 12–24 hours of exposure to cold.
Chilblains typically cause a burning and itching sensation in the extremities, which gets worse and intensifies going into a warm room.
The skin of the affected area may swell and turn red or dark blue. In severe cases, the surface of the skin may break and sores or blisters can develop.


It's important not to scratch the skin as it can break easily and become infected.
- Common signs and symptoms include:
- A burning sensation on the skin
- Small red, blue or white swollen patches
- Intense itching
- Pain and tenderness in the affected area
- Dermatitis in extremities
- Possible blistering of affected area
- Dry skin, leading to splits and cracks
- Possible econdary infection
- Digital ulceration, in severe cases only
Chilblains last about seven days and usually get better within a couple of weeks on their own if the patient avoids exposure to cold, without permanent damage. Some cases may flare up whenever the weather gets cold.
Causes of chilblains
The exact reason chilblains occur is not well-understood but cold (specifically, exposure to both mild nonfreezing cold and humidity), is the direct requirement for the development of symptoms. Chilblains are the result of an abnormal vascular reaction (arteliolar and venular constriction) to prolonged exposure to temperatures above freezing point when damp or humid conditions coincide, followed by too rapidly rewarming (e.g. warming cold hands in front of a fire or heater).On rewarming, venular constriction predominate on arteriolar constriction with exudation of fluid into the tissues. Minor trauma or tight clothing may also predispose to symptomatic pernio lesions in otherwise appropriate weather conditions.
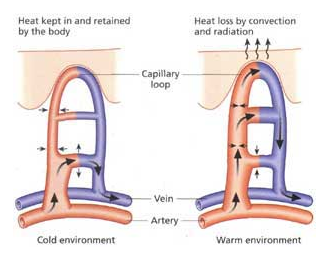
When the skin is cold, the farthest blood vessels (small arteries and veins) (hands, feet, tip of the nose) near its surface get narrower (constriction). If the skin is then exposed to sudden warmth, in rewarming of cold skin, small blood vessels closest to the skin cannot handle their sudden expansion that occurs more quickly than nearby larger blood vessels can handle, resulting in a "bottleneck" effect and the blood leaking into nearby tissues causes inflammation, swelling and itching.
Our skin acts like a thermometer and helps sense the temperature outside and inside our body; it makes sure we are always perfectly warm at 37° Celsius (98.6° Fahrenheit) . When the temperature outside lowers, our skin tries to preserve our internal heat by sending signals to our farthest blood vessels in our hands, feet, and tip of our nose telling those vessels to squeeze tight; this slows the flow of hot blood to our most distant tissues and retains heat toward the center of our body. In chilblains, those distant “shut-off” areas begin to react abnormally to the lack of blood flow. The blood vessels closest to the skin surface, and with the least blood, wage a full inflammatory response asking the body to pay attention to them. Instead of helping the situation, the inflammation actually leads to the destruction of blood vessels and real damage to the skin above them.
Pernio can be idiopathic but chronic pernio may be secondary to various systemic diseases
A history of chilblains may be suggestive of a connective tissue disease. Chilblains in infants, together with severe neurologic disease and unexplained fevers, can be seen in Aicardi-Goutieres syndrome, a rare inherited condition.
- Chronic pernio may be secondary to various systemic diseases as follows:
- Chronic myelomonocytic leukemia
- Viral hepatitis
- HIV infection
- Rheumatoid arthritis
- Anorexia nervosa: low body mass index may predispose to pernio.
- Dysproteinemias
- Macroglobulinemia
- Cryoglobulinemia, cryofibrinogenemia, cold agglutinins
- Antiphospholipid antibody syndrome
- Raynaud disease
- Celiac disease
Perniosis occurring in lupus erythematosus is known as chilblain lupus erythematosus or Hutchinson’s lupus.
- Factors that may contribute to increase risk of chilblains include:
- Skin exposure to cold. Any skin that is regularly exposed to damp or draughty conditions and then rapidly warmed may develop chilblains.
- Female. Women are more likely to get chilblains.
- Low body weight or poor nutrition. People who are underweight (about 20 percent less than are expected for their height) have an increased risk of chilblains.
- Where a person lives. Oddly, chilblains are less likely in areas which are drier and colder because the living conditions and clothing used in these areas are more protective against cold. But then, if an individual lives in an area with high humidity and low, but not freezing temperatures, the risk of chilblains is greater.
- Time of year. Chilblains are more common from November to April. Chilblains often disappear completely in the spring.
- Poor circulation. People with poor circulation tend to be more sensitive to changes in temperature, making them more susceptible to chilblains.
- Diagnosed with Raynaud’s phenomenon. Having been diagnosed with Raynaud's phenomenon. An individual with Raynaud's phenomenon which is another cold-related condition that affects the extremities, are more susceptible to chilblains. Both conditions can cause sores, but Raynaud's causes different types of color changes on the skin.
- Diagnosed with Lupus Erythematosus. Lupus erythematosusis an autoimmune connective tissue disease whose in which the clinical presentations range from a skin rash unaccompanied by extracutaneous stigmata to one comprising progressive multisystem disease
- Shoes are ill-fitting. Chilblains can also develop on areas of the feet that are exposed to unusual pressure, such as tight shoes
- Smoking. Nicotine constricts blood vessels.
Complications of chilblains
Chilblains can cause complications if the skin is blistered or scratched.
- The possible complications of chilblains include:
- infection
- ulcers
- permanent discolouration of the skin
- scarring of the skin
Besides being painful, infections are potentially life-threatening if left untreated.
Laboratory Studies
Investigations for chilblains are generally not indicated but if the history or examination raise the possibility of a systemic cause or if the person's history does not indicate excessive cold exposure, the following laboratory tests may be needed:
- CBC count and sedimentation rate (to rule out associated leukemia).
- Antiphospholipid antibody panel (patients with chilblains shows an increased incidence of antiphospholipid antibody syndrome).
- Cryoglobulins, cryofibrinogen, and cold agglutinin testing (they should be considered in a patient with chronic chilblains).
- Antinuclear antibody (ANA)( to rule out lupus erythematosus).
- Serum protein electrophoresis (SPEP) and quantitative immunoglobulins (dysproteinemias and macroglobulinemia, can cause increased serum viscosity and may be associated with chilblains).
Histologic Findings
Diagnosis of chilblains is usually based on clinical findings. Biopsy (punch biopsy) may be indicated if the diagnosis is in doubt or to rule out other inflammatory processes in difficult chronic cases.
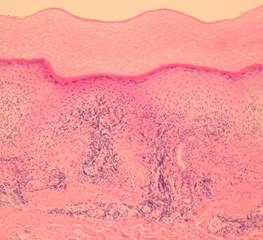
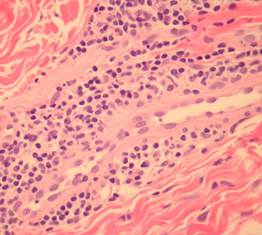
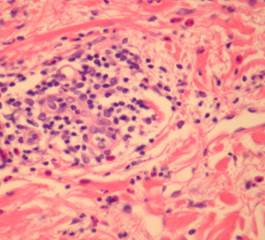
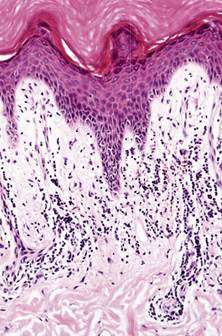
- The four characteristic findings are
- scattered necrosis of individual keratinocytes,
- marked subepidermal oedema,
- perivascular lymphocytes
- lymphocytic vasculitis.
Histologic sections show a dense superficial and deep perivascular lymphocytic infiltrate (1) within the dermis and sometimes extending to the subcutis (2,3)(“fuffy edema” of vessel walls) with intense subepidermal oedema. In early lesions there may be numerous eosinophils (4). There may be well established fibrinoid change and thrombosis.
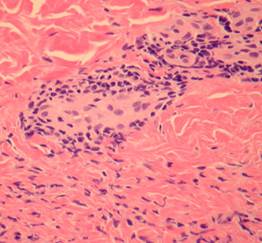
In lupus erythematosus vacuolation of the basal layer is more common, mucin is usually increased in the dermis and the lupus band test (that is IgG at the dermo-epidermal junction) is positive. The presence of antinuclear antibodies favours a diagnosis of lupus
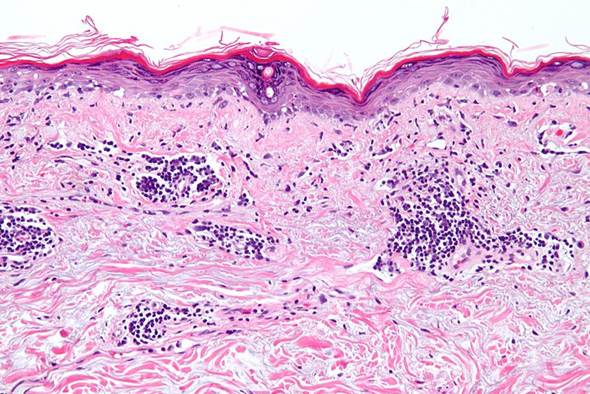
Skin biopsy revealed proliferation of thick-walled blood vessels and edema of the dermal papillae. The lumens of these vessels were narrow. There was a superficial and deep perivascular lymphocytic infiltrate in the upper dermis. The epidermis revealed only mild spongiosis and focal lymphocytic exocytosis without necrotic keratinocytes
Immunofluorescence study shows IgG deposits at two different places: the first is a bandlike deposit along the epidermal basement membrane ("lupus band test" is positive); the second is within the nuclei of the epidermal cells (antinuclear antibodies are present).
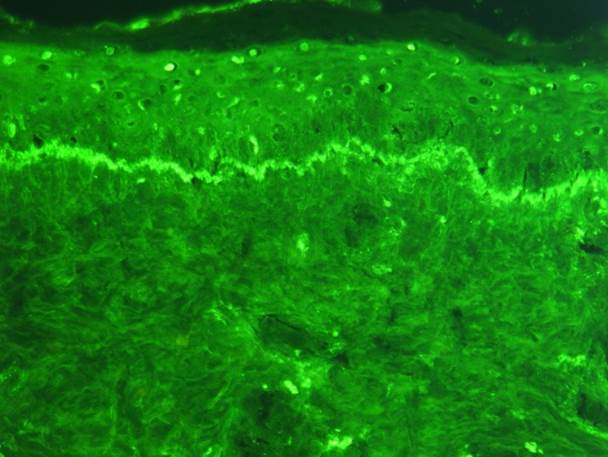
Lymphocytic vasculitis and interface changes are more common in chillblain lupus than in idiopathic chilblains. A positive antinuclear antibody test favours chilblain lupus erythematosus.
Variants of chilblains
Variants include the following:
- Kibes (equestrian cold panniculitis): Erythrocyanotic plaques occur on the upper lateral thighs of women who ride horses. Histology is characterized by an intense perivascular infiltrate extending into subcutaneous fat.

- Chilblain lupus erythematosus: Violaceous "pernio" plaques appear prominent over dorsal interphalangeal joints, often with positive antinuclear antibody (ANA) or rheumatoid factor (RF). Histologic and immunofluorescent evidence of lupus is present in the skin lesions. Half of the patients have associated facial discoid lupus lesions, and 15% develop systemic lupus.




- Drug-induced pernio: Sulindac-induced cases have been reported.
Differential Diagnoses
The differential diagnosis of chilblains is broad and depends on the stage of the disease at presentation as well as the appearance and location of the lesions.
A variety of conditions have been described as predisposing patients to pernio:
- systemic lupus erythematosis,
- cryopathy or connective tissue disease (with loss of seasonal patterns)
- chronic myelogenous leukemia(CML)
- polycythemia vera,
- thrombotic or embolic phenomena
- Raynaud's syndrome,
- atheromatous embolization,
- pernio sarcoid,
- erythromelalgia,
- vasculitis,
- peripheral artery disease,
- purple toe syndrome from anticoagulant therapy
- CA-MRSA (Community-Associated Methicillin-resistantStaphylococcus aureus)
- erythema induratum,
- nodular vasculitis,
- erythema nodosum,
- cold panniculitis,
- atheromatous embolization,
Among children, the presence of cryoproteins, such as cold agglutinins and cryoglobulins, has been reported in association with pernio. Excessive cold exposure and parental neglect have also resulted in pernio.
Among adolescents, pernio has been seen in association with anorexia nervosa.
Among children another entity to consider is microgeodic disease, consisting of chilblain-like appearance, tenderness of digits, and radiographic findings of patchy osteoporosis; radiographic evaluation may be considered to help confirm this diagnosis.13
Among adults, pernio has been reported in association with systemic lupus erythematosus, lupus anticoagulant, anticardiolipin, and antiphospholipid antibodies, chronic myelocytic leukemia, metastases from carcinoma of the breast, and reaction to medication.
Cryoglobulinaemia, cryofibrinogenae mia and other hypercoagulable states should be considered, especially in atypical or refractory cases.
Raynaud's phenomenon
In the presence of an acute exacerbation, the major alternative in the differential diagnosis of chilblains is Raynaud's phenomenon. Raynaud's phenomenon is an abnormal vasoconstrictive response to cold; however, spasm or closure of cutaneous arteries results in sharply demarcated cutaneous pallor and cyanosis, followed by erythema, and the response is of far shorter duration (hours rather than days).


Chilblain lupus erythematosus
Chilblain lupus erythematosus (also known as "chilblain lupus erythematosus of Hutchinson) is a rare cutaneous form of lupus erythematosus characterized by painful bluish-red papular or nodular lesions of the skin in acral locations—including the dorsal aspects of fingers and toes, heels, nose, cheeks, rims of ears, and, in some cases, also knees. It is precipitated by cold and wet exposure at temperatures <10°C.
The onset of the skin lesions was in early childhood, and, in most patients, the lesions tended to improve during summer.
Biopsy results help differentiate chilblain from chilblain.



Kaposi sarcoma
Kaposi sarcoma should be suspicious when violaceous nodules or patches develop on the palms or soles of elderly patients. Some cases may mimic chilblains because of the exclusive localization of the violaceous nodules and patches on the handswith worsening of the lesions with cold. Nevertheless, the avoidance of cold not only did not improve the condition, but the eruption gradually became more extensive.

Acrocyanosis
Acrocyanosis is a symmetric painless, discoloration of different shades of blue in the distal parts of the body (fingers and toes and, in some cases, the entire hands and feet). Less frequently the nose tips and ears may be affected.
Acrocyanosis is differentiated from Raynaud because of symmetry, relative persistence of the skin color changes and absence of paroxysmal pallor. Unlike Raynaud phenomenon, patients with acrocyanosis do not experience a return to baseline circulation between vasospastic episodes. Although cold may exacerbate cyanosis, rewarming does not return circulation to baseline. It is aggravated by cold exposure and it is frequently associated with clamminess and hyperhidrosis of hands and feet.
Acrocyanosis is considered primary (idiopathic, essential) when no apparent cause can be determined. It is considered benign and no specific treatment is required because may spontaneously resolve, withoput evolving into serious disease. Primary acrocyanosis commonly appears in adolescence and more likely female patients under the age of 30 years.
Secondary acrocyanosis is a manifestation of various diseases and in some cases may be the first sign of the primary disorder which may become fully manifest with the passage of time.
It is often marked by asymmettry, variability of manifestations, associated with pain and tissue damage,


Cold urticarial
Cold urticaria is a skin reaction to physical exposure to cold objects as cold water, air, or ingestion of cold liquids and foods.. Skin, within 2-5 minutes after contact with cold, develops reddish, itchy welts that last for 1-2 hours. The severity of cold urticaria symptoms varies widely. Some people have minor reactions to cold, while others have severe reactions. Swimming in cold water is the most common cause of a whole-body (systemic) reaction. This could lead to very low blood pressure, fainting, shock and even death.

- Some condition that have been associated with secondary cold urticarial:
- Lymphosarcoma
- Viral hepatitis
- Infectious mononucleosis
- Chickenpox
- Chronic lymphocystic leukaemia
- Cryoglobulinemia
- Hypothyroidism
- Leukocytoclastic vasculitis
- Drugs like penicillin, oral anticoagulants and antifungal
- Infective mononucleosis
Cold urticaria can be diagnosed by applying an ice cube against the skin of the forearm for 1-5 minutes. A distinct red swollen rash should develop within minutes in the area exposed to the cold-stimulation test if a patient has cold urticaria.


Conditions associated with blue toes (due to arterial insufficiency or drug-induced)
- Atheromatous embolization.
- Thrombotic embolization.
- Peripheral arterial disease.
- Blue toe syndrome — adverse effect associated with warfarin treatment (rare).
Conditions associated with erythematous, nodular, and ulcerative lesions

Erythema nodosum
Erythema nodosum (EN) is an acute, nodular, erythematous eruption that usually is limited to the extensor aspects of the lower legs.
May be associated with fever, arthralgias, and malaise. May be primary or secondary to an underlying cause ( Bacterial infections, fungal infections, drugs, entropathies, Hodgkin disease, sarcoidosis, behcet disease, pregnancy)
Lesions are painful but do not ulcerate.
Cold panniculitis

Cold panniculitis (CP) is characterized by localized, erythematous nodules with well-defined margins usually limited to areas exposed to the cold. Nodules, firm or hard and cold and painful, are raised slightly above the skin line.
Cold panniculitis results from a cold injury to adipose tissue: it’s not due to dermal vascular injury as perniosis
Cutaneous distribution in children characteristically is on the face (cheeks and forehead), Skin color changes are red or violet.
In women who are obese, cutaneous distribution characteristically is on the buttocks, thighs, arms, and under the chin (areas poorly protected from the cold). Thigh lesions, in particular, overlap with perniosis.
Lesions may be reproduced by applying an ice cube to the skin.
Histology reveals fat necrosis.


Erythema multiforme
It is an immune-mediated disease.
It usually presents with mildly itchy, pink-red blotches, symmetrically arranged and starting on the extremities. It often takes on the classical "target lesion" appearance, with a well-defined pink-red ring around a pale center
Lesions are usually found on hands and feet but can also appear on oral, conjunctival, and genital mucosae.
Sarcoidosis
Lupus pernio is a confusing term; it is related to neither pernio nor to lupus erythematosus, but is the most characteristic cutaneous lesion of sarcoidosis. Skin lesions are generally in the form of infiltrated nodules or plaques, with shiny skin changes varying in colour from red to purple (usually dusky-red. Scarring is uncommon. They appears on the nose, cheeks, lips, ears, fingers, toes.
The large nodular type usually involves the face, hands, and trunk, whereas the small nodular type predominantly affects the extensor aspects of the limbs.

Nodular vasculitis
Generally affects women 30–40 years of age.
Develops as recurrent, painful, nodular lesions of the calves which do not generally ulcerate.
There is no relationship to cold exposure.
There is no associated tuberculosis infection.

Erythema induratum (Bazin's disease)

A cutaneous reaction to tuberculosis.
It is initiated or exacerbated by cold weather, and typically presents as one or more recurrent erythrocyanotic nodules or plaques on the calves of women.
The nodules may progress to form indurations, ulcerations, and scars
A tuberculin skin test is usually positive.
Quantiferon test commonly positive.
Treatment
Although chilblains are uncomfortable, they do not usually cause any permanent damage. They will usually heal on their own if any further exposure to the cold is avoided.
Avoiding chronic exposure to cold temperatures is the first step in treating pernio.
Keeping both the affected extremities and the core body dry and warm are essential in preventing pernio.
- Patients should have some self-help measures, including:
- wearing appropriate insulated, loose-fitting clothing ,
- ensuring home temperature be well heated
- avoiding exposure to damp, cold environments
- keeping always feet dry (moisture enhances cold injury)
- keeping active
- stopping smoking
- limiting alcohol intake
- avoiding tight-fitting shoes and boots
- wearing thick socks and shoes
- wearing gloves
If the skin gets cold, it's important to warm it up gradually. Heating the skin too quickly, for example by placing the feet in hot water or near a heater, is one of the main causes of chilblains.
Treatments options require therapeutic agents that increase digital blood circulation (vasodilatory effects). They are prescribed (under GP supervision) until warm weather returns and restarted in the autumn as prophylaxis.
The calcium channel blocker, nifedipine (10 mg three times daily or 20 mg twice daily) is very effective in increasing the rate of resolution of existing chilblains and if it is taken during the winter can prevent their appearance because stop them to develop. Blood pressure should be monitored at the start of treatment and at return visits.
Amlodipine (2.5-5 mg once daily) may be used as an alternative to calcium channel blockers. The long half-life and consequent once daily dosing of this drug are beneficial when chronic therapy is required
Nicotinamide (500 mg three times daily) may be useful alone or in addition to calcium channel blockers but flushing and palpitation are problematic.
Hexylnicotinate (2% cream applied three times daily) may be useful for patients who are, intolerant of, or unwilling to take oral medication.
Alternative options are erythema doses of ultraviolet light (UVB) to affected areas 2 to 3 times a week at the start of winter may prevent the development of lesions.
In order to prevent infection, if the skin has broken, management should include cleaning and shielding the wounds.
Corticosteroid creams may help to relieve swelling as well as itching.
Prevention
Chilblains can easily be prevented not exposing or limiting to expose the skin to cold temperature for long time. All exposed skin should be well covered to keep the entire body warm all times in cold climate.
Prevention strategy include exercising regularly to improve peripheral circulation. Exercise to improve circulation do plenty of exercise at least four times a week; this helps maintain good circulation Keep active. This helps improve your circulation. Have some gentle exercise, like walking, every day to improve peripheral circulation. If you are outside in the cold, keep active to improve your circulation Exercise to improve circulation do plenty of exercise at least four times a week; this helps maintain good circulation Keep active. This helps improve your circulation.
- Suggestions include:
- Avoid long periods of exposure to cold or damp weather.
- Avoid cold exposure whenever possible
- Cover all exposed skin as completely as possible when going outside in cold weather
- Wear warm clothes and insulate your hands, feet and legs. Wearing long johns, long boots, tights, leg warmers or long socks will help. If you get cold feet in bed, wear a pair of clean socks.
- Dress warmly. Try wearing two thinner layers instead of one thick layer. Wearing several loose layers is ideal to trap body heat.
- Avoid wearing tight-fitting socks that cut off the blood circulation.
- Use woollen or cotton socks to allow your feet to ‘breathe’
- Wear clothing that protects your feet, hands and ears from the cold.
- protect the nose by wrapping something like a scarf around part of the face. Keep head and ears warm by wearing a hat and scarf.
- Wear several warm layers of clothing, which trap body heat more efficiently than one bulky layer.
- Wear gloves to protect fingers and hands
- Wear appropriate socks and shoes to insulate the feet.
- Use warm footwear.
- Keep hands and feet warm.
- Make sure you keep your hands, feet and face warm.
- Make sure your shoes are comfortable and well fitted. Avoid tight shoes and boots as these can restrict the circulation to toes and feet. Warm your shoes on the radiator before you put them on. Make sure damp shoes are dry before wearing them. Wear shoes with a thicker sole to prevent heat loss.
- Dry feet thoroughly after showering or bathing.
- See a podiatrist for regular professional treatments.
- Keep your home and workplace comfortably warm.
- Avoid rapid changes in temperature. After being out in the cold, Do not directly overheat chilblains (for example using hot water) do not heat the skin quickly with hot water bottles, etc. Gradually warm up. When coming back from the cold, do not expose susceptible areas to sudden warmth (a gradual process is better).If the skin is exposed to cold weather, it is useful to rewarm the skin gradually since any sudden rewarming of cold skin will only worsen chilblains.
- Avoid tight fitting socks/shoes
- Wear adequate clothing (should be loose and in layers to trap body heat.to keep the body warm.
- Place cotton wool between the toes to improve circulation
- Protect the head and ears by wearing a hat and scarf.
- Dress in layers of warm clothings
- Stop smoking.Nicotine causes the blood vessels to constrict (get narrower), which can make chilblains worse. Cease smoking.
- If you are diabetic, give yourself regular foot checks (or ask someone else to do this). Diabetics may not be able to feel their feet and could have septic chilblains without realising.
- Keeping your affected skin warm, but away from sources of heat
- Healthy diet. In cold weather, eat at least one hot meal during the day. This will help warm your whole body. In cold weather, eat regular meals and include at least one hot meal a day.
- Keep your skin moisturised. Moisturise your feet regularly. This stops them drying out and the skin cracking.
- Drink hot drinks to keep your entire body warm.
- Avoid alcohol before going out in snow.
- Avoid medicines that may constrict blood vessels, such as caffeine and decongestants.
