BALANOPOSTHITIS
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
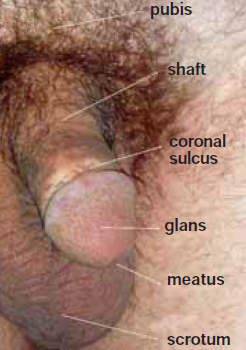
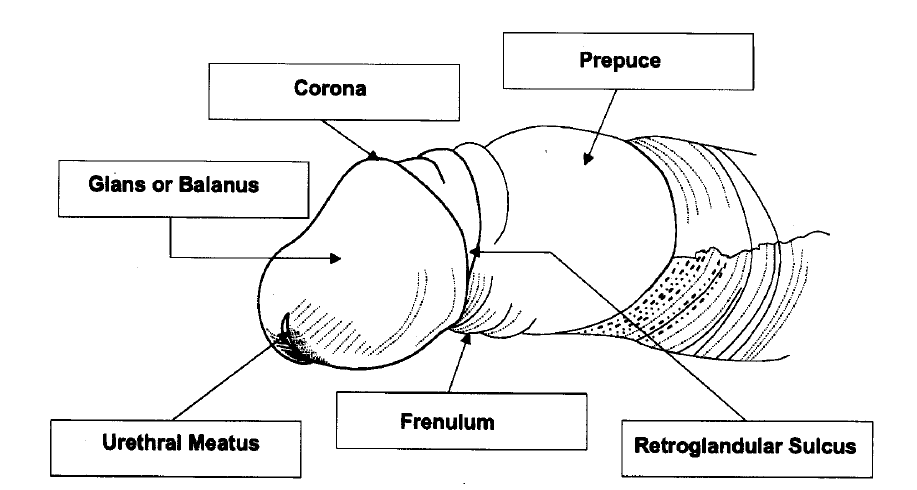
Balanoposthitis is an inflammation of the glans penis (balanitis) together with inflammation of the foreskin (posthitis). Balanitis is a descriptive term covering a variety of unrelated conditions, the appearances of which may be suggestive but should never be thought to be pathognomonic
Balanoposthitis occurs over a wide age range and is more common in uncircumcised penis (about 3:1over circumcised men) possibly as a result of poorer hygiene and aeration or because the constantly covered skin is hotter and moister, and thus receptive to bacterial and fungal (i.e. candida) overgrowth and prone to irritation and inflammation by smegma (although not shown to be a direct cause of non specific balanoposthitis).
Balanoposthitis may have multicausal origin: infectious, mechanical/traumatic, contact dermatitis.
The majority had an infective cause (yeast, fungus, bacteria, or virus infection), although a greater proportion with mild disease had irritant or mechanical reasons for the inflammation.
Candidal infection appears to be the most frequently diagnosed (Candida species accounted for 30% of the causative organisms,). Other organisms that have been identified include Bacteroides, Gardnerella, and beta-hemolytic streptococci (beta-hemolytic streptococci accounted for 13% of the causative organism).
In one third of the patients, a specific cause could not be established even after clinical examination and microbiologic and serologic tests had been performed.
Older men often have other etiologies, including intertrigo, irritant dermatitides, or other fungal infections.
Balanitis which persists and in which the cause remains unclear warrants biopsy.
CLASSIFICATION OF BALANITIS IN ADULTS
A common way to classify balanitis by differential diagnosis is into infectious and noninfectious causes:
Infectious
-
Fungal infection (Candida albicans, Pityriasis versicolor)
-
Anaerobic infection (Bacteroides species)
-
Aerobic infection (Group B β-hemolytic streptococci)
-
Mycobacterial infection (Tuberculosis)
-
Protozoal infection (Trichomonas vaginalis)
-
Spirochetal infection (Syphilis, Lepra)
-
Viral infection (Genital herpes, Human papillomavirus infection, Bowenoid papulosis)
Noninfectious
-
Pemphigus (various types)
-
-
Erythoplasia of Queyrat
-
Bowen disease of the penis
-
Bowenoid papulosis
-
-
Pseudoepitheliomatous, micaceous and keratotic balanitis (PKMB)
-
(in Reiter's syndrome)
-
Dermatologic disease in male genitalia
-
Psoriasis vulgaris
-
Lichen ruber planus
-
Seborrhoeic dermatitis
-
pemphigus
-
Physiological curiosity
INFECTIOUS BALANITIS
Fungal infection
Candidal balanitis is considered to be the most common cause of balanitis and is due to infection with candidal species, usually Candida albicans. It is generally sexually acquired. Symptomatic infection is more common in the uncircumcised male. Significantly more of the female partners of men carrying yeasts were found to have candidal infection.
But infection may occur without sexual contact, usually in the presence of diabetes (of which it may be the presenting symptom) or after the use of oral antibiotics.
Signs are blotchy erythema with small eroded white papules, or generalized erythema of the glans and/or prepuce with a dry glazed appearance.




In diabetic patients the presentation may be more severe with oedema and fissuring of the foreskin, which may become non-retractile.



Symptoms are of soreness and/or burning and itching of the penis.
Diagnosis may be on clinical appearances alone, but subpreputial culture confirm it.
Treatment of Candida infection can be topical or oral antifungals. Because in sexual partners there is a high rate of infection, they should be screened
Pityriasis versicolor
This condition is caused by the yeast Malassezia furfur. Genital involvement is uncommon and presents as a discrete, circinate, finely scaling hypopigmented areas on the glans which fluoresce in Wood's light. The lesions can be treated with topical antifungals.

Gardnerella vaginalis
It may represent the milder end of the spectrum of anaerobic infection.The symptoms of pure Gardnerella vaginalis balanitis are milder than those in anaerobic infection: diffuse, macular erythema and pruritus of the glans meatus and coronal sulcus, irritation of the prepuce, , and a fishy-smelling subpreputial discharge. Urethral discharge is minimal, with a characteristic fishy odor when present. Coinfection with anaerobes is common.
Metronidazole is currently the first-line drug of choice (400mg twice daily for 1 week) with saline subpreputial washes. Patients are advised strongly not to drink alcoholic beverages while taking this medication and for at least 3 days after finishing the treatment because mixing metronidazole with alcohol can cause severe, unpleasant side effects, such as abdominal pain, cramps, nausea and vomiting, headachesand flushing.
Aerobic infection
Diagnosis is obtained by subpreputial culture. The clinical appearance is of nonspecific erythema with exudates (erythematous moist balanitis) or without it.
Sexual transmission is unclear. The mode of transmission seems to be autoinoculation from other sites, but not excluded following fellatio.
Streptococci Group B streptococci are strongly associated with balanitis. Group A haemolytic streptococci have been reported as causing it. Staphyloccocus aureus has infrequently been reported as causing a balanitis
Penicillins or cephalosporins are effective in treatment.
Mycobacterial infection
Penile tuberculosis is very rare. In most cases, the lesion appears as a superficial ulcer on the glans or around the corona (the most common part rubbed during sexual contact or with infected clothing). Rarely the lesion may be present as a solid nodule. It may be primary or secondary to pulmonary tuberculosis.
Tuberculosis of penis may affect the skin, glans, penis frenulum, or cavernous bodies. Destruction of the glans may be caused by the disease process and advanced cases may present with erectile failure due to tuberculous caveronositis. The female partner should always be evaluated for genital tuberculosis. For differentiation from carcinoma penis, histopathological examination is essential. IVU should be done to exclude the upper renal tract tuberculosis.
The primary cases occur as
-
a complication of ritual circumcision. In ritual circumcision, the operator (with open pulmonary tuberculosis) sucks the circumcised penis as a haemostatic and styptic measure. After the turn of the century this act was practically eliminated.
-
during coital contact with the disease already present in the female genital tract (the bacilli are inoculated into abrasions caused by vigorous sexual act since the normal mucosa is highly resistant to tuberculosis)
-
from contact with infected underwear clothings
-
by reinoculation of the male partner through his own infected ejaculate as vagina is particularly resistant to tuberculosis.
-
complication of intravesical instillation of immunotherapy (BCG vaccine) for carcinoma urinary bladder
Secondary penile tuberculosis
can occur along with evidence of active pulmonary tuberculosis elsewhere. Sometimes concomitant diabetes leads to such an atypical manifestation of tuberculosis.
Tb of the penis may present as one of the following:


-
Small ulcer on glans penis/corona (painless or painful).
-
Multiple small ulcers on the penis.
-
Small reddish nodules,
-
A gradually enlarging ulcer on the glans penis.
-
indurated plaques,
-
deep-seated papules,
-
nodules coalescing to form cords rendering a granulomatous clinical,
-
A nodule on the penis.
-
An induration of the penis.
-
A swelling of the penis.
-
Erectile failure.
Leprosy involvement of the glans penis has been reported in leprosy alone and in association with penis tuberculides.
Protozoal infection
Trichomonas can cause a sexually acquired superficial erosive balanitis which may lead to phimosis. It may be associated with other infections. This condition responds well to treatment with metronidazole.
Amoebic infection

Amoebic infection of the genitalia in both sexes is an extremely rare and unusual ectopic site. The classic presentation is of a painful penile ulcer, which progresses rapidly with a foul-smelling hemo-mucopurulent exudetes, and necrotic slough. Amoebic ulcers are serpiginous, with a well-demarcated (often undermined) edges with a raise erythematous rym. Pain is extremely intense and inguinal lymphadenopathy is usual present. The mode of infection is by direct inoculation during vaginal or anal intercourse with a person suffering from amoebic dysentery.
Genital amoebiasis should be considered in the differential diagnosis of benign and malignant ulcers of the penis. The best differentiating feature between penile cancer and amoebic ulcer appears to be the absence of pain in patients with cancer.
Diagnosis can be made on the typical appearance of the ulcer, its acute onset, rapid progression, and associated intense pain. Wet mount microscopy of ulcer exudates demonstrates trophozoites.
Treatment is with metronidazole (two weeks course) and antibacterial agents to prevent secondary infection. A two-week course of metronidazole shows with dramatic regression of the ulcer in 1 week and complete regression in 2 weeks. In case of massive destruction of the penis, surgical intervention may be necessary.
Spirochetal infection

Syphilitic balanitis is usually characterized by a primary chancre. Multiple circinate irregular may be present in the late primary or early secondary stage.
Non syphilitic spirochaetes Ulcerative balanitis has been associated with infection by non-syphilitic treponemes of the borrelia group.
Viral infection
Genital herpes is a common and highly contagious infection. This infection is usually caused by the herpes simplex virus-2 (HSV-2) or the herpes simplex virus-1 (HSV-1) . HSV-2 has been traditionally more associated with genital infections than HSV-1 but this last is increasingly associated with genital infection . Primary Herpes simplex is rare and can be asymptomatic. The clinical features and course of primary genital herpes caused by both HSV-1 and HSV-2 are indistinguishable, Symptomatic primary genital herpes has an incubation period of 3-7 days (range, 1 day to 3 weeks). And it is characterized by severe and prolonged systemic and local symptoms. Primary herpes can cause a necrotising balanitis, with necrotic areas on the glans Local symptoms include pain, itching, dysuria, and urethral discharge, and tender lymphadenopathy.
It may be associated with fever, headache, malaise, and myalgia (prominent in the first 3-4 days)., The ulcerative lesions persist from 4-15 days until encrusting and reepithelialization occur.

More commonly people suffer of recurrent genital herpes ( more common with HSV-2). Recurrent genital herpes is preceded by a prodrome of tenderness, pain, and burning at the site of eruption that may last from 2 hours to 2 days recurrent genital herpes presents as 1 or more patches of grouped vesicles on the shaft of the penis, prepuce, or glans.
Human papillomavirus (HPV) (Genital warts)
HPV is a viral infection. It’s a growth on the skin that look like tiny bump or group of bumps in the genital area around the penis. The lesions might be small or large and
can vary in number, shape (flat, raised, or like a cauliflower), color (skin-colored, red, pink, grey, or white), firmness, and symptoms (none, itchiness, or pain).
The warts may go away, or stay the same, or grow in size or number.
The most common location for genital warts in men is under the foreskin of an uncircumcised penis, or on the shaft of a circumcised penis. Warts can also appear on the testicles, groin, thighs, or around the anus.


NONINFECTIOUS BALANITIS
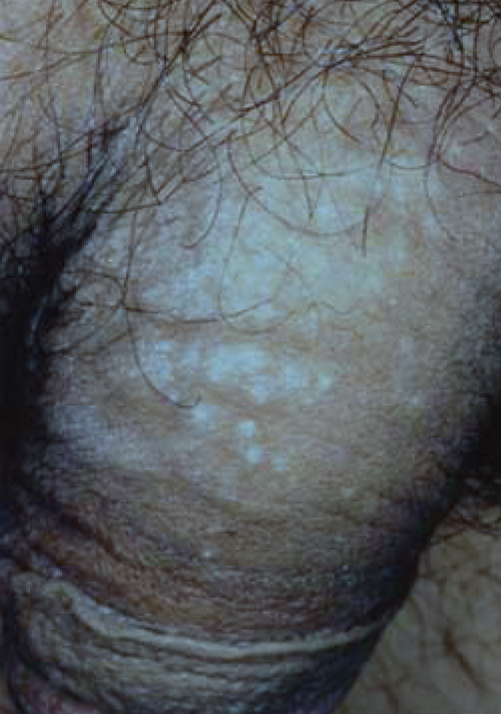
Balanitis xerotica obliterans
This is a descriptive term for a scarring balanitis which is most commonly caused by lichen sclerosus et atrophicus, an inflammatory skin condition possibly of autoimmune pathogenesis. Other causes are rare and include pemphigus vulgaris and chronic nonspecific bacterial balanitis.
The condition affects all ages. The main symptoms are itching, soreness, splitting, haemorrhagic blisters, dyspareunia pain, irritation, disturbance of sexual function, or urinary symptoms (including obstruction but may be asymptomatic)
The clinical appearance is of white plaques on the glans, often with involvement of the prepuce which becomes thickened and non-retractile. There may be haemorrhagic vesicles, purpura and rarely blisters and ulceration.


Possible incoming changes include blunting of the coronal sulcus, phimosis or wasting of the prepuce, and meatal thickening and narrowing


Complications may be phimosis, urethral stenosis, malignant transformation in penile squamous cell carcinoma.
The course is chronic and relapsing, and although it may sometimes arrest, the areas of atrophy do not regress.
Plasma cell balanitis (Zoon)
First described by Zoon in 1952, Zoon balanitis is a disease of older men who are uncircumcised.
Clinical appearance is variable and includes well circumscribed, orange-red areas with a characteristic glazed appearance on the glans with multiple pinpoint redder spots (cayenne pepper spots).
Sometimes pain, irritation and discharge occur.
In cases of diagnostic uncertainty penile biopsy should be performed. The appearances of premalignant disease (erythoplasia of Queyrat) can be very similar. Histological appearances are characterized by epidermal atrophy, loss of rete ridges, "lozenge keratinocytes" and spongiosis. A predominantly plasmacytic nature of the infiltrate is found subdermally.
The course is chronic and poorly responsive to topical treatment but it can resolve completely on circumcision


Pre-malignant conditions
There are three clinical presentations of penile carcinoma in situ (PCIS) included in undifferentiated PeIN (Penile intraepithelial neoplasia).
-
Erythroplasia of Queyrat
-
Bowen disease of the penis
-
Bowenoid papulosis
All are associated with high risk HPV types including 16.
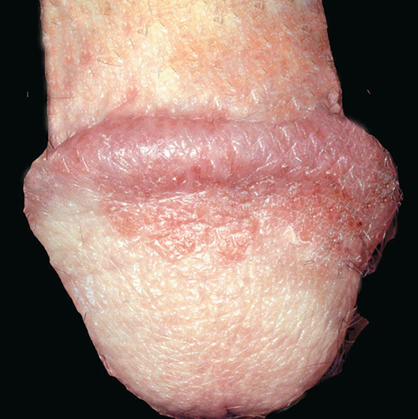
Erythroplasia of Queyrat
Erythroplasia of Queyrat is a premalignant condition (carcinoma in situ) affecting the penis, usually the glans, prepuce or meatus. It was described by Queyrat in 1911. It has a characteristic appearance: red, velvety, well circumscribed area (single or multiple) with sharp margins and a granular surface on the glans. If lesions are keratotic or indurated, it suggests the development of frank squamous cell carcinoma.
There are various treatment options. Circumcision is recommended.
Follow up after treatment is obligatory because of the possibility of recurrence. It is estimated that up to 30% of cases progress to invasive cancer.


Bowen Disease of the penis

Bowen disease, is a growth of cancerous cells that is confined to the outer layer of the skin. It is a clinical presentation of in situ squamous cell carcinoma, that, Very occasionally, can progress into an invasive squamous cell carcinoma (the rate of progression to invasive carcinoma was shown to be similar to that of erythroplasia of Queyrat).
Bowen disease is generally seen in elderly uncircumcised men and presents as a sharply marginated, erythematous, scaly patch or plaque (from millimeters to centimeters in diameter) on the shaft of the penis.

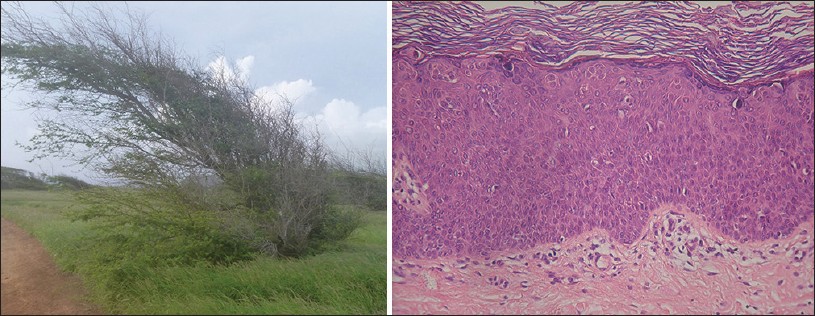
Bowen’s disease is usually diagnosed by its appearance, but a biopsy may be necessary for a definitive diagnosis. The histopathology is similar to that of bowenoid papulosis and erythroplasia of Queyrat, showing features of in situ carcinoma, such as full-thickness epithelial atypia with disorderly maturation of the epidermis or lack of maturation, nuclear atypia, dyskeratotic cells, and atypical mitoses. This overall appearance in the epithelium of Bowen's disease is referred to as "windblown appearance The underlying dermis typically displays a lymphohistiocytic inflammatory infiltrate. Evidence of tumor invasion into the underlying dermis is absent.

Pigmented Bowen's disease (PBD) is a variant of squamous cell carcinoma in situ (less than 2% of cases of Bowen's disease). It is characterized by a sharply demarcated, irregular pigmented plaque with a scaly or crusted surface.
Bowenoid papulosis

Bowenoid papulosis is a rare form of penile intraepithelial neoplasia. It presents as single or multiple small, red, flesh-coloured but often pigmented discrete papules with a flat-to-verrucous surface or coalesce into large plaques,. The lesions most commonly appear on the shaft of the penis.
Most cases of Bowenoid papulosis appear to run a benign course but a small percentage may transform into invasive squamous cell carcinoma.
They may also be present on other parts of the genitals as well as in and around the anus. The condition is usually symptomless but occasionally lesions may become inflamed, itchy and painful.




Bowenoid papulosis may regress spontaneously and conservative treatment is often considered.
The histological differentiation of bowenoid papulosis and Bowen’s disease is difficult.
In Bowenoid papulosis the stratum corneum and granular cell layer often contain small inclusion-like bodies. Inclusion bodies are deeply basophilic, rounded and sometimes surrounded by a halo.
These inclusion bodies, together with the numerous metaphase mitoses, are the features that can suggest a diagnosis of bowenoid papulosis rather than Bowen’s disease.
Pseudoepitheliomatous, micaceous and keratotic balanitis (PKMB)
PKMB is a rare condition of the glans penis affecting the elderly uncircumscribed men, first described by Lortat-Jacob and Civatte in 1960. PKMB presents as a thick hyperkeratotic plaque with thick adherent micaceous scaling. PKMB is generally asymptomatic but irritation, burning sensation, fissuring or maceration may be associated. Thickness of the plaque may sometimes be so much so that the lesion appears as a penile horn. Hyperkeratotic plaques involving perimeatal skin may cause multiple urinary streams on micturition giving an appearance of a "watering-can penis"
PKMB may be considered as lesion with low-grade malignant potential, prognostically. PKMB may be histologically classified a squamous hyperplastic lesion that stain negatively for immunohistochemical markers of high grade penile intraepithelial lesions (p16/p53)
The clinical course of PKMB is chronic and associated with recurrences despite initial response to treatment which, most of the times, is partial.
Differential diagnoses include penile horn, penile psoriasis (early plaque stage), giant condyloma, verrucous carcinoma, erythroplasia of Queyrat, SCC, and keratoacanthoma.

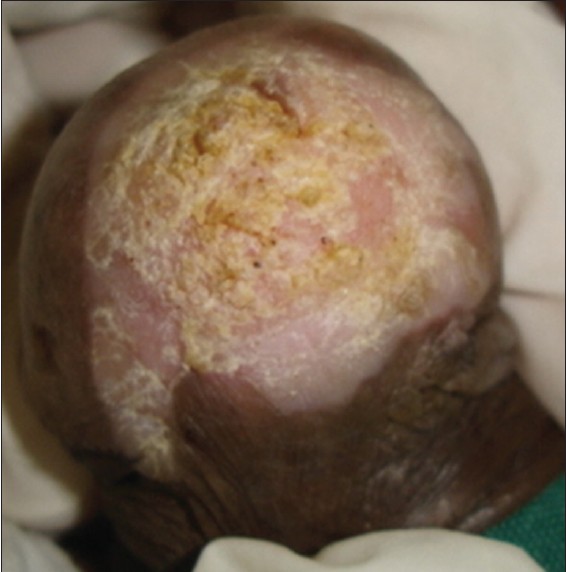
The choice of treatment is generally guided by the stage of the disease.: treatment options include topical measures like 5-FU, podophyllin resin, steroids and physical measures like cryotherapy, radiotherapy, and surgical excision.
Circinate balanitis


It is an inflammatory condition that occurs in Reiter’s disease/reactive arthritis. Reiter syndrome (Rs)/Reactive arthritis (ReA) is a painful form of inflammatory arthritis triggered by an infection of certain bacteria or virus (trigger) in intestines (gastrointestinal-GI), genitals or urinary tract (GU). in genetically predisposed individuals.
Circinate balanitis, consists of small shallow painless ulcers of the urethral meatus or the glans penis. The condition is characterized by circinate or gyrate graysh white areas that grow centrifugally and coalesce to form larger "geographic" areas with a white margin: they eventually cover the entire surface of the glans penis. The penile shaft and scrotum can be involved. On an uncircumcised penis, the lesions typically remain moist; on a circumcised penis, they may harden and crust, causing pain and scarring in 50% of patients.
Circinate balanitis may occur with or without other features of Reiter's syndrome.
Fixed drug eruptions (FDE)

Fixed drug eruption is an uncommon condition related to ingestion of a causative agent that may occur via any route, including oral, rectal, or intravenous.
The lesions usually develop within 30 minutes to 8 hours of taking the drug
The major categories of causative agents of fixed drug eruption include
-
Analgesics (Paracetamol /phenacetin and other pain killers)
-
Muscle relaxants (e.g. hyoscine butylbromide)
-
Sedatives (including barbiturates, benzodiasepins and chlordiazepoxide)
-
Antiepileptics
-
Phenolphtalein
-
Antibiotics (especially tetracyclines and sulphonamides including cotrimoxazole)
-
Nonsteroidal anti-inflammatory agents (including ibuprofen),
-
Dapsone
-
Acetylsalicylic acid/aspirin
although other agents, numerous nutritional supplement, over-the-counter medication, or, rarely, food (eg, fruits, nuts cashews and licorice) have also been reported as causative agents.
After sensitization to a drug, FDE appears as a solitary or multiple lesions (macules or plaques) usually well demarcated and erythematous. Sometimes may develop bullae with subsequent ulceration.
The lesions typically recur at the same anatomic sites after exposure to the same drug.
Most lesions will fade spontaneously without treatment, but may leave an area of residual hyperpigmentation. Occasionally treatment with topical, or rarely systemic steroids may be required, if the lesion is severe.


Irritant and allergic balanitis
Many cases are non-specific and no aetiological agent can be found. In contrast to allergic penile dermatitis, irritant lesions of this region occur more frequently.
A history of fluctuating episodes (particularly if symptoms are persistent or recurrent or unresponsive to treatment), of atopy illness, of frequent daily genital washing with soap were predictive of irritant balanitis. More severe reactions have been seen with topical agents: dequalinium is known to cause a necrotic balanitis.


Use of emollient creams and restriction of soap washing alone control symptoms satisfactorily.
Balanitis as an allergic reaction is very uncommon. There is a wide spectrum of clinical manifestations : varying from erythema, microvesiculation, erosions, crusts to oedema of the whole penis.
Contact allergic dermatitis of the penis may develop after hand to penis contact, sexual intercourse. The source of the allergen may be the condom material or rubber diaphragms, the lubricant (paraben preservatives) or the feminine hygiene deodorant prays and douches, or lubricants containing propylene glycol.
Patch testing and avoidance of the precipitant is required.
Dermatologic disease in male genitalia
Many dermatological conditions may have a predilection for the male genitalia: Psoriasis, seborrhoeic dermatitis , lichen planus, pemphigus.
Psoriasis
Psoriasis in genital region often shows only change in appearance; sometimes soreness or itching can occur.
In the circumcised male psoriasis on the glans is similar to the appearance to the condition elsewhere with red scaly plaques. In the uncircumcised scaling is lost and the patches appear red and glazed.
The key to the diagnosis is to look for the presence of psoriasis elsewhere. However some patients have psoriasis confined to the penis
Biopsy may be necessary particularly in the glazed pattern of psoriasis which can look similar to premalignant conditions and other inflammatory conditions.
Lichen Planus
Lichen planus (LP) is an inflammatory autoimmune disease in which the immune system becomes overactive and causes inflammation. It affects both glabrous and mucosal skin.
In general, LP affects the most middle-aged to older men in the age group of 30-60 years.
LP of Penis can occur on the glans on the prepuce or on the penile shaft, as a single lesion or multiple lesions (Purplish well demarcated plaques pink, shiny, flat-topped papules) in a ring-like pattern (annular pattern). The size of the lesion may vary from 1 mm to 10 mm.


Lichen Planus has a slow onset; it may take days and weeks for the signs and symptoms to develop.

It is not a sexually contracted disease.
Usually asymptomatic and non-itchy in many individuals, in some people mucosa become red and raw (erosive lichen planus): it is very painful, making sexual intercourse unconfortable. It may also result in severe itch.
After onset of the condition, the lesions may last months and sometimes even for years.
Seborrhoeic dermatitis


Seborrhoeic dermatitis is a common, chronic or relapsing form of eczema that mainly affects the scalp, eyebrows, nasolabial crease. Genital involvement can occur.
Pemphigus

Pemphigus vulgaris is a chronic, autoimmune bullous disease affecting themucosae and skin. The mucosa of the oral cavity is most frequently involved, but the glans penis may be affected. It is characterized by coalescing erosions of the glans penis and sulcus coronaries with a whitish macerated appearance with delicate fissures.
But pemphigus vulgaris may have the clinical picture of balanitis xerotica obliterans, and the rare variant of pemphigus vegetans characterized by papillomatous and vegetative lesions



Many are the possible differential diagnoses for long-standing penile erosions: infectious etiologies (herpes simplex virus, syphilis, candidiasis, and mycobacterial infection), fixed drug eruption, erosive lichen planus, genital aphthosis of Behçet's disease, and premalignant and malignant conditions like plasma cell balanitis, Paget's disease, erythroplasia of Queyrat and squamous cell carcinoma.
Physiological curiosity

Sebaceous gland hyperplasia (Fordyce spots)
Sebaceous glands are found in association with hair follicle. Sometimes they also be found ectopically without hair follicle as on the glans or shaft of the penis. They appear as harmless, small solitary or, more frequently numerous yellowish or white papules. Not require treatment except if they are of cosmetic concern.
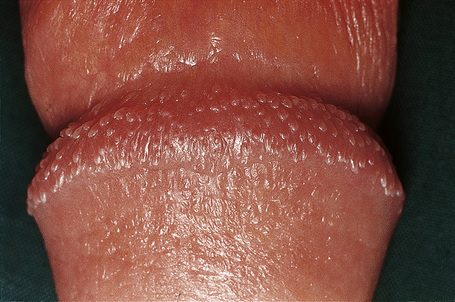
Pearly penile papules
Pearly penile papules (PPP) (less commonly referred as “Hirsuties papillaris penis”) are asyntomatic angiofibromas typically found as one or several rows of small, flesh-colored, smooth, dome-topped to filiform papules distributed circumferentially along the corona or sulcus of the glans penis.
Because of their anatomic distribution, pearly penile papules are noted only in men, after puberty, in their second or third decades of life.
It is a harmless, benign, physiological condition They are not contracted or spread through sexual activity and their appearance is unrelated to sexual activity or standards of personal hygiene.
PPP are asymptomatic and persist throughout life; however, they gradually may become less noticeable with increased age.