Acquired bilateral nevus of Ota-like macules (ABNOM) (Hori’s nevus)
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
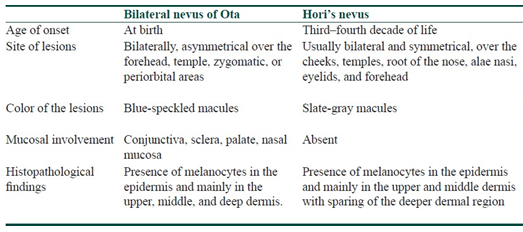
Acquired bilateral nevus of Ota-like macules (ABNOM) also known as Hori′s nevus is an acquired dermal melanocytoses most commonly seen among people with dark skin, especially in women of Asian descent in the twenties. It also goes by the synonyms "Nevus fusco-caeruleus zygomaticus and Acquired circumscribed dermal facial melanocytoses."
Hori's nevus, was originally described as acquired bilateral nevus of Ota-like macules (ABNOM), by Hori et al. in 1984. They reported 22 cases of blue-brown and/or slate-gray small patches of the face, occurring on both sides of the forehead, temple, eyelids, malar area, alae of the nose, and root of the nose in middle-aged Japanese women. The age of onset ranged from 19-69 years.
Initially the lesions consist of aymptomatic multiple, symmetrical speckled macules with a a mixed hue of brown, slate-gray, blue-black color occurring bilaterally on the malar areas. The number of spots on each malar region varies and some of the guttate macules over time progress to form confluent, large macules.


Less commonly multiple sites may be involved including the root and alae of the nose, the temples, the upper eyelids, without ocular or mucosal pigmentation. In these areas the lesions are often homogeneous and slate gray in color, and appear as large confluent macules like Mongolian spots rather than in a speckled pattern.




Unlike nevus of Ota, there is no pigmentation of the conjunctiva, the buccal or the palatal mucosa.
Summarizing Hori’s nevus is characterized:
- Symmetrical, bilateral distribution
- Mild and brown-dominant small spots scattered on the lateral sites of the forehead, upper and lower eyelids, and the malar area;
- Lack of mucosal pigmentation;
- Late onset in adulthood (20-30 years)
- A marked female preponderance
- A family history.
Hori’s nevus can occur simultaneously with other pigmentary abnormalities such as melisma, frekles, solar lentigines, and nevus of Ota.
PATHOGENESIS
The pathogenesis of this condition is unknown, but several theories have been put forward. These include
(a) dropping off of epidermal melanocytes;
(b) migration from follicular bulb melanocytes;
(c) reactivation of pre-existing misplaced latent dermal melanocytes from faulty migration during embryological development, triggered unknown event (dermal inflammation, UV radiation, or hormonal changes in pregnancy?).
Two hits are needed for the development of ABNOM:
- the first, the ectopic placement of inactive, poorly melanized dermal melanocytes at birth or soon thereafter
- the second, the activation of these melanocytes in response to ultraviolet exposure, excessive sex hormone, chronic inflammation such as atopic dermatitis, or other unknown triggers.
HISTOPATHOLOGY AND ELECTRON MICROSCOPY
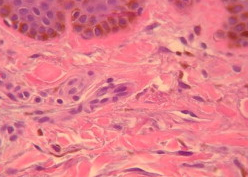
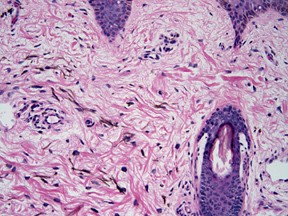
Histopathologically, the epidermis appears normal. The main changes are in the middle and upper dermis.
There are elongated, slender, irregularly shaped pigment bearing (identified as actively melanin-synthesizing dermal melanocytes) arranged predominantly as single units between collagen bundles of the dermis, particularly within the papillary and upper reticular dermis. Their long axis is along the collagen fibers and does not disturb the normal architecture of the skin. The pigment bearing cells contain many singly dispersed melanosomes in stage II, III, IV of melanization. These structures are 0.3x0.5 um2 in diameter and are surrounded by an extracellular sheath.
This condition is characterized by prominent epidermal hypermelanosis together with Numerous pigment-laden dermal macrophages.
Variations in color (brown, gray, blue) are due to the varied proportion of pigmented cells in the epidermis and dermis.
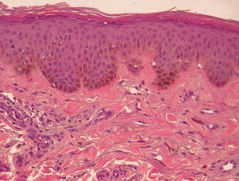
In nevus of Ota, dermal melanocytes are seen to involve the deeper reticular dermis as well.
DIFFERENTIAL DIAGNOSIS
Oriental patients in the thirties often present with a mixed picture of lentigines, freckles, melasma, post-inflammatory hyperpigmentation and Hori's nevus, with difficulty to tell the exact nature of some of the individual pigmented spots clinically. Confusion also arise with dermal melasma.
For this reason it is usefull to have a good, clinical differential diagnosis.
Freckles/Ephelides

Freckles (ephelides is the medical term) are small flat brown marks arising on the face and other sun exposed areas. They are most often seen in fair skinned people, especially those with red hair, but they are an inherited characteristic that sometimes affects darker skin types as well. The colour of ephilides is due to localised accumulation of skin pigment (melanin) in the skin cells (keratinocytes).
Their appearance varies seasonally, being darker, more prominent and more confluent in the summer, when cells called melanocytes produce more melanin when exposed to the sun (melanin then diffuses into the surrounding keratinocytes).
Frekles become fainter in the winter as the keratinocytes are replaced by new cells.
In contrast, the symmetrical type of nevus of Ota or Sun's nevus appears mainly on the zygomatic area without seasonal changes.

Lentigines
Also known as senile lentigo or solar lentigo, age spots, lentigines are the most common benign sun-induced lesion.
They appear as small, pigmented flat or slightly raised, spots with a clearly defined edge that is surrounded by normal-appearing skin.
Single or multiple, they occur in sun-exposed areas (face, arms, dorsa of the hands, and upper part of the trunk).
The lesions are usually brown, but the color may range from yellow-tan to black. Older lesions are often dark brown or brownish black.


Lentigines are common in those with fair skin but are also frequently seen in those who tan easily or have naturally dark skin.
The spots initially are smaller than 5 mm in diameter and may evolve slowly over years, increasing in number and in size, eventually coalescing to form larger patches. But they may appear suddenly.They tend to persist for long periods and don't disappear in the winter (though they may fade).
The surface of the lesions is either flat or depressed, and it may be split by fine wrinkles.

Although these lesions are most common in individuals aged 30-50 years, they are now seen in younger individuals because of their increased exposure to sun tanning and the use of artificial sources of UV light. Although they are often called liver spots, they are not a manifestation of systemic disease.
Lentigines are due to localized proliferation of melanocytes
Multiple lentigines on the face in a child may be the most prominent manifestation of the LEOPARD syndrome.
Melasma
Melasma(brown skin) (also known as Chloasma faciei) is a chronic skin discoloration that results in symmetrical, blotchy, brownish facial pigmentation. Although it can affect anyone, melasma is particularly common in women, especially pregnant women and those who are taking oral or patch contraceptives or hormone replacement therapy (HRT) medications.

Melasma usually appears in people that tan well or have naturally brown skin


(Fitzpatrick skin types 3 and 4).
Melasma presents as macules (freckle-like spots) and larger flat brown patches with an irregular border, on both sides of the face.

There are several distinct patterns.
- Centrofacial pattern: forehead, cheeks, nose and upper lips
- Malar pattern: cheeks and nose
- Lateral cheek pattern
- Mandibular pattern: jawline
- Reddened or inflamed forms of melasma (also called erythrosis pigmentosa faciei)
- Poikiloderma of Civatte: reddened, photoaging changes seen on the sides of the neck, mostly affecting patients older than 50 years
- Brachial type of melasma affecting shoulders and upper arms (also called acquired brachial cutaneous dyschromatosis).
Melasma is classified into epidermal (skin surface), dermal (deeper) and mixed types by Wood lamp examination (this lamp emits black light-UVA1).
Epidermal melasma is characterized by
- Well-defined border
- Dark brown colour
- Appears more obvious under black light
- Responds well to treatment
Dermal melasma
- Ill-defined border
- Light brown or bluish in colour
- Unchanged under black light
- Responds poorly to treatment
Mixed melasma
- The most common type
- Combination of bluish, light and dark brown patches
- Mixed pattern seen under black light
- Partial improvement with treatment
In melasma, the periorbital area is never affected and the involvement of the alae of the nose and root of the nose alone is very rare, although distribution of the pigment is mostly symmetrical and similar to that of Hori's nevus.
Melasma is usually well demarcated and uniform in color, but is rarely mottled. In Hori's nevus, however, the border is less clear, the color contains a blue or purple-brown tint, and the pigmentation is sometimes speckled.
Melasma is exacerbated by sun exposure and lightened by long-term sun protection, whereas Hori's nevus is rarely influenced by sun exposure.
Symmetrical type of nevus of Ota (bilateral nevus of Ota).
In 1939, Professor Ota’s pupil Tanino classified his original 26 cases into four types: (1) mild, including two subtypes: (a) orbital, and (b) zygomatic; (2) moderate; (3) intensive; and (4) bilateral (5–8% of patients).

In 1965, Hidano classified bilateral type of nevus of Ota into two types:
- symmetric
- asymmetric.
The asymmetric type is usually moderate to severe, and the extent or severity of pigmentation is different between the right and left side of the face.
Characteristic features of the symmetrical type are:
- symmetric distribution;
- mild and brown–dominant small spots scattered on lateral sites of the forehead, upper and lower eyelids, and malar area;
- no mucosal pigmentation;
- rare and slight ocular pigmentation;
- late onset;
- a marked female preponderance;
- some family history.
This type of nevus of Ota appeared after 20 years of age in 1⁄3 of the patients and was frequently misdiagnosed as ephelides.
Hidano proposed, therefore, that it is a new clinical entity with slight differences from classical nevus of Ota.
Nevus fuscocaeruleus zygomaticus (Sun’s speckled nevus)
In 1987, Sun described an acquired (not congenital) speckled discoloration of the skin of the face principally in the zygomatic area. It becomes apparent between 8 and 40 years, mainly in females, with a positive family history in 18% of the cases.
This nevus is similar to the symmetrical type of nevus of Ota proposed by Hidano (clinical manifestations and family history) with the difference in the age of onset.
Nvus of Sun would be an acquired form of nevus of Ota, whereas nevus of Hori is a form of acquired bilateral nevus oof Ota-like lesion.
Nevus of Sun occupies a smaller area than nevus of Ota and is distributed in the territory of the zygomatic branch of the trigeminal nerve instead of the ophthalmic branch of nevus of Ota and the skin discoloration is not homogeneous, but speckled. Moreover nevus of Sun never involves eye structure.

Infraorbital ring-shaped melanosis (dark rings under the eyes)
“Dark rings under the eyes”, is an expression used to indicate pigment macules under the eyes which are prominent and appear as a condition of general fatigue, especially with regards to insufficient sleep. Similar fluctuation of color tone is frequently noticed in patients with nevus of Ota during or before menstruation, after insufficient sleep, and⁄or when the patients are tired or sick.
Some patients with unilateral nevus of Ota complain of homogeneous pigment macules on the infra orbital area on the opposite side of the face after significant improvement of the unilateral nevus by Q–switched ruby laser (QSRL). A skin biopsy of the pigmented macule on the infra orbital area indicated that dark rings under the eyes are caused by dermal melanocytosis.
The possible cause of dermal melanocytosis change day by day is the thickening of the dermis caused by edema, leading to an enhanced incidence of diffuse light reflection from the pigments, which then results in increased darkness of the skin.


Periorbital ring–shaped melanosis (Panda–like nevus of Ota)
“Periorbital ring-shaped melanosis (Panda–like nevus of Ota)” indicates homogenous pigment macules on the bilateral periorbital area caused by dermal melanocytosis. This condition has been frequently observed among Indians.
Riehl’s melanosis

Riehl’s melanosis is a facial pigmentation described for the first time during World War I, in the spring of 1917, by a dermatologist, Gustav Riehl, who observed some patients with striking dark-brown to grayish-brown pigmentation most pronounced on the lateral aspects of the face and neck and primarily concentrated on the forehead, ears, temple, and zygomatic regions.
Riehl speculated that the hyperpigmentation occurred because of some nutritional alteration that he attributed to wartime conditions.
Riehl's melanosis is today almost synonymous with pigmented contact dermatitis of the face. The commonest cause has been sensitizing chemicals in cosmetics, including aniline dyes, formaldehyde,geraniol, lemon oil, and the optical whitener tinopal.
The pigmentation varies dependent upon the causal agent and can be brown, slate-gray, gray-brown, red-brown, or blue-brown.
Histologically, the lesions were marked by a dense inflammatory cell infiltrate in the superficial dermis admixed with melanophages.
THERAPEUTIC APPROACH
Hori's nevus is particularly challenging to treat because the melanocytes are located perivascularly (leading to a higher likelihood of postinflammatory hyperpigmentation after laser therapy), and the frequent association with melasma (possible associated presence of epidermal pigmentation). However the use of pigment-specific lasers namely the Q-switched Nd: Yag laser (1064 nm), Q-switched alexandrite laser (755 nm), and Q-switched ruby laser (694 nm) are reported as effective treatment with good-to-excellent clearing.
Prior epidermal ablation with a carbon dioxide laser has been found to increase the therapeutic efficacy of pigment-specific lasers.
Hypopigmentation, erythema, and hyperpigmentation are nevertheless possible complications.
Dermabrasion using the coarse diamond fraise tip has also been found to be cost effective with good cosmetic results.
