PROGRESSIVE MACULAR HYPOMELANOSIS (PMH)
Nummular and confluent hypomelanosis of the trunk, cutis trunci variata, Creole dyschromia, idiopathic macular hypomelanosis of the melanodermic halfcast of Guillet-Hélénon, idiopathic multiple large macule hypomelanosis
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
Progressive macular hypomelanosis (PMH) is a condition of unknown etiology characterized by macules that are:
-
hypopigmented (whitish)
-
round-to-oval
-
poorly defined
-
predominantly located on the posterior and anterior trunk
-
simmetrical distributed
-
asymptomatic
-
non scaly
-
gradually increasing in number
-
with a tendency to coalesce
-
less commonly located on the neck and areas close to the extremities
- without previous history of inflammation, infection, or injury.


There is no signs of inflammation on the borders of the lesions, no atrophy or scarring, no facial involvement. Family members did not show any similar skin manifestations.
It is a common dermatosis in different continents such as Africa, Europe, Asia and the Americas. The term "progressive macular hypomelanosis" was first employed by Guillet et al. in 1988 to describe this hypopigmentation primarily whithin young women with Fitzpatrick skin types IV-VI resident in France, originating from the French Caribbean and West Indies, of mixed racial background (Black/Caucasian).
Although more common in darker skin types, PMH has been reported in patients with skin types I-III in the United States, northern Europe and throughout Asia under various names including cutis trunci variata in Venezuela, dyschromia creole in the French West Indies, progressive and confluent hypomelanosis of the melanodermic metis, nummular and confluent hypomelanosis of the trunk in the Netherlands, and progressive macular confluent hypomelanosis and idiopathic multiple large macule hypomelanosis in the United States. PMH mainly affects adolescents and young adults, with a more prevalence in females.
PMH was initially thought to exclusively affect patients with Fitzpatrick skin types V and VI from tropical and subtropical climates. However, in the following years there were reports of the disease also in lighter skin patients (Fitzpatrick types II-IV). The absence of patients over 40 years of age suggests that PMH may be a self-limiting disease. The progression of the disease is variable, ranging from months to years. Diagnostic criteria of PMH:
-
clinical features (asymptomatic, acquired, nonscaly, confluent hypopigmented macules on the trunk)
-
presence of red follicular fluorescence restricted to hypopigmented spots that is absent in adjacent normal skin
Several differentials have to be ruled once PMH is considered:

Pityriasis alba (dry white patches) is a benign condition of children and adolescents, which is frequently located on the face presenting hypopigmented patches with a slight overlying scaliness and elevated borders. Pityriasis alba is basically an eczematous type of disorder, with seasonal variation (exacerbation in the summer and the winter), often associated with atopy. Skin lesions often present a preceding inflammatory phase. Spongiosis is the most consistent finding on histological examination.

Pityriasis versicolor is an asymptomatic superficial fungal infection typically affecting the upper trunk (less often the neck and face).
It is characterized by multiple hypo- or hyperpigmented round to oval minimally scaling macules, coalescing into patches without evidence of erythema. This condition is caused by the fungus known as Malassezia furfur, more specifically the dimorphic lipophilic yeast forms Pityrosporum ovale and Pityrosporum orbiculare. Tinea versicolor is commonly seen in adolescents and young adult (likely due to liphophilic nature of the fungus and therefore predilection for people with increased sebaceous activity) during the summer months when unaffected skin tans normally, but the lesions remain relatively hypopigmented because the organism produces an inhibitor of tyrosinase, which prevents tanning.It is sometimes seen in younger children, more commonly on the face. The disease less often affects older patients.

Postinflammatory hypopigmentation is usually more localized than PMH and occurs in the aftermath of dermatitis or inflammatory conditions such as lichen planus, eczema, atopic dermatitis, psoriasis. So, in absence of these preceding condition, post-inflammatory hypopigmentation can be ruled out.

Idiopathic guttate hypomelanosis. is an acquired, benign disorder of both sexes (but most commonly is a complaint of middle-aged, light-skinned women, with a history of a long-term sun exposure) going along with multiple tiny confetti-like hypopigmented macules on extremities, expecially on calves and shins.

Pityriasi rotunda affects both men and women, can be familial, with endemic areas in some geographical areas, such as the isle of Sardinia in Italy, Japan, south of Africa, and the Antilles. It is considered a rare variant of ichtyosis and is characterized by round or polycyclic, uniformly scaling,sometimes hypopigmented patches. Patients may have summerremissions and winter exacerbations.

Hypopigmented macules in post-kala-azar dermal leishmaniasis (PKDL). It is an unusual dermatosis occurring between 6 months and 5 years following an attack It is characterized by hypopigmented macules, erythema, and nodules. Histopathology is very important in ruling out the differentials. The parasite demonstration in dermal lesions is the gold standard diagnostic criteria for PKDL. The skin smears from depigmented macules did not show any amastigote.

Hypopigmented micosis fungoides is a rare variant of mycoses fungoides first described by Ryan et al. in 1973. It is characterized by multiple hypopigmented, well-demarcated non-scaly, asymptomatic macules and patches over the trunk, buttock and proximal.The disease is rare in white caucasian but has predilection for dark-skinned individuals of young age (mean of 29 years)

Leprosy. The lesions are usually asymmetric with almost complete anesthesia (loss of sensation).

Guttate pityriasis lichenoides chronica (PLC), may have a history of hypopigmented macules on the trunk, legs, and arms associated with a few skin-colored to yellow papules with a collarette of scale. Potassium hydroxide examinations of several lesions is, of course, negative for fungal elements. Histology confirm the diagnosis showing a superficial dermal infiltrate, focal parakeratosis, preservation of the granular layer, and focalvacuolar interface changes Necrotic keratinocytes at the dermoepidermal junction are not tipically present.
The clinical history (no sign or symptoms of atopy, scrapings for potassium hydroxide -KOH- examination and gram stain negative for fungi and bacteria, normal sensibility on the macules, no preceding inflammation), and eventually the histological findings should reveal the correct diagnosis. The exact pathogenesis of progressive macular hypomelanosis is unknown. In 2004, Westerhof et al proposed that PMH is caused by Propionibacterium acnes.
This suggestion was based on the observation that Wood’s lamp examination in a dark room produced a red follicular fluorescence of the hypopigmented spots, which is absent in normal adjacent skin. This was further substantiated by culturing P acnes from pilosebaceous ducts of lesional skin. The hypothesis was formulated that P acnes produces a factor that interferes with melanogenesis, leading to hypopigmented macules.
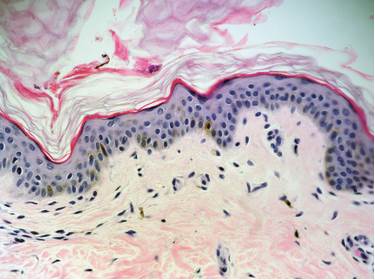
PMH is characterized histologically by diminished pigment (a lower melanin content with no reduction in the number of melanocytes) in the epidermis than in normal skin and a normal-looking dermis.
There are no significant inflammatory infiltrates or epidermotropism. Periodic acid-Schiff staining failed to reveal fungal elements.
In 1983 Zaynoun et al. reported, under the name of extensive pityriasis alba (EPA), nine cases of an acquired hypopigmentation occurring in dark-skinned young adult females from the Lebanon.
The clinical features are similar to PMH ( the sex ratio, age of occurrence 15–25 years, seasonality -end of summer-, skin phototype of the affected patients III–V, widespread and symmetrical involvement of the skin of the trunk with numerous, round, non-scaling hypomelanotic patches without a preceding inflammatory phase and with a long-lasting duration, decrease epidermal melanin on histological examination, absence of spongiosis, reduced number of active melanocytes and a decrease in the number and size of melanosomes in the affected skin on ultrastructural studies). No atopy or associated pathologies or familial cases were reported.
