ACTINIC GRANULOMA
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
Actinic granuloma (AG) is a skin disorder characterized by annular (ring-shaped), asymptomatic plaques, similar to those observed in granuloma annulare (GA), on sun-exposed sites (head, neck and hands). It was first described in 1975 by O'Brien (“O'Brien granuloma”)
Actinic granuloma begins as flesh-coloured or pink papules (small bumps) which coalescence into annular plaques, ranging from 1 to 10 cm in diameter. The placques have slightly raised borders and an atrophic, hypopigmented central area.

Its pathogenesis is unknown; however, the most widely accepted hypothesis suggests that solar radiation and chronic sun exposure are the triggering factors (the reaction is confined to the superficial dermis, corresponding to the zone of solar elastosis) and that the altered elastic fibers (the specific target of the disease) induce an inflammatory response that causes granulomas.
The postulated mechanism behind the actinic damage hypothesis is that solar-damaged elastic fibers are weakly antigenic and result in a cell-mediated immune response with a predominance of CD4 lymphocytes. This immune response is thought to be an attempt to repair the actinically damaged skin but results in granulomatous inflammation instead.
Support for this hypothesis comes from
- the sun-exposed distribution of the disease,
- the presence of CD4 cells,
- the presence of giant cells that appear to be ingesting the elastic fibers
Others Authors argue that elastic fiber destruction is caused by the granulomatous inflammation itself. So the debate is if granulomas are the consequence of or actually the cause of the damaged elastic fibers.
There has been also much controversy regarding whether O’Brien’s actinic granuloma is a specific, separate nosological condition, since some authors (Ragaz and Ackerman) consider it to be a simply granuloma annulare occurring in sun-exposed areas of the skin.
The two dermatoses are often clinically similar, but certain histopathological characteristics can classify actinic granuloma as a separate condition.
In the case of AG:
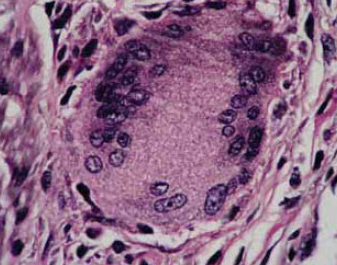
- uniform presence of multinucleated giant cells with fragmented elastotic material in its interior
- loss of elastic fibers ormarked elastophagocytosis, on sun damaged skin
- mild scarring
- no necrobiosis
- no increased dermal mucinwithin zones of granulomatous inflammation
- granulomata are sarcoidal and interstitial,
- no palisading granulomata
- granulomata are confined to the superficial dermis at solar elastosis level.
- trend toward a greater number of eosinophils
On the other hand, in GA:
- granulomata are usually palisading or interstitial
- no sarcoidal granulomata
- granulomata typically involve both the superficial and deep dermis
- mucin is present.
- not appreciable loss of elastic fibers or elastophagocytosis
AG suggest an inflammatory response directed toward smaller materials, such as individual altered elastic fibers that are more readily destroyed to the point where they are no longer visible by light microscopy.
In GA, the occurrence of palisading granulomata suggests an inflammatory response to persistent and relatively large aggregates of material, as a reaction to nodules of altered collagen. The reaction is expected to occur throughout the superficial and deep dermis without regard for location of the collagen.
Thus the identification of a palisading or sarcoidal pattern of granulomatous inflammation may be helpful in distinguishing these two entities.
But as an entirely interstitial pattern can be found in both conditions, the other histologic features must be used in the distinction.
Treatment of actinic granuloma is difficult because, nevertheless several different therapeutic options, the result is not certain and sometimes little if at all:
- topical or intralesional corticosteroids (into the raised edge)
- acitretin,
- isotretinoin,
- cycklosporine,
- chloroquine,
- pentoxiphylline,
- cryotherapy,
- retinoid psoralen + UVA (RePUVA)
- methotrexate.
But some patients experience spontaneous resolution of the lesions. To prevent development of new lesions, patients should avoid sun exposure and use sunscreen.
