LICHEN PLANUS PIGMENTOSUS INVERSUS
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
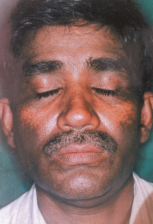
Lichen planus pigmentosus (LPP), first described by Bhutani et al. is a rare chronic variant of lichen planus (LP). It is usually characterized by the presence of dark-brown macules or papules (but pigmentation may vary from slate grey to brownish-black) mostly in sunexposed areas or the face and neck. But few cases present mottled hyperpigmentation, zosteriform, arcuate, reticular, linear patterns.
It was originally described in Indian populations and in the Middle East and generally stars in the third or fourth decade of life.

LPP is uncommon in the classical form in Europe where arises in light-skinned people, predominantly in non sun exposed, flexural and intertriginous areas and is referred to as LPP inversus.
Lesions are generally bilaterally simmetrical.
It has an insidious onset and has a chronic course with gradual extension in size and deepening in colour. The lesions are usually asymptomatic and not associated with pruritus or pain.
The scalp, mucosa and nails are not involved, as palms and soles.
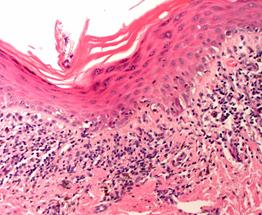
Histopathology shows presence of basket weave horny layer, minimal change in epidermal thickness with vacuolar degeneration of basal cell layer in the epidermis.
At the dermoepidermal junction there is a band-like or perivascular lymphohistiocytic inflammatory infiltrate. In the dermis is present pigment incontinence with scattered melanophages.
The cause of LPP is unknown, but the histologyc findings suggest that immunologic mechanisms (cell-mediated immune reactions involving T lymphocytes) play a central role in the pathogenesis and LPP probably represents a lichenoid reaction to an unknown agent or stimuli.
The differential diagnosis includes
-
Drug induced dermatosis
-
Acanthosis nigrigans
-
Ashy dermatitis
-
Mycosis fungoides
-
Contact and occupational dermatosis with hyperpigmentation
These can be differentiated clinically, by history and histologically.
There is no proven effective, specific treatment for LPP. Topical steroids and tacrolimus, an immunosuppressive agent, currently used in the topical management of atopic dermatitis and several other inflammatory skin disorders, because of its immunosuppressive activities by inhibiting T-cell dependent immune functions, have been tried in the treatment of LPP with variable success in isolated cases.
