ACTINIC KERATOSES
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
DEFINITION
Actinic keratoses (also known as solar keratosis) are rough, scaly erythematous patches or spots on the skin that develop on sun-damaged skin typically in elderly patients with lighter skin types from years of exposure to the sun. They are most commonly found on areas of skin typically exposed to the sun ( face, lips, ears, back of the hands, forearms, scalp or neck). Actinic keratoses enlarge slowly, take years to develop (usually first appearing in older adults) and usually cause no signs or symptoms other than the lesion on the skin
OVERVIEW
Actinic keratoses (Ak) (also called "solar keratoses" and "senile keratoses") represent focal areas of abnormal keratinocyte proliferation and are considered premalignant lesions with low individual potential to malignant transformation (less than 1 in 1000 per annum) (pregression to squamous cell carcinoma - SCC) and a high spontaneous regression (in the order of 15-25% for Aks over 1-year period)
Aks are often recognized by touch rather than sight. In fact Aks start out as small barely perceivable rough spots of skin that feel similar to rubbing sandpaper. The color ranges from skin-colored to pink to reddish brown.
Most often, they appear as multiple discrete, flat or elevated, thickened, scaly or warty, keratotic lesions. Lesions typically have an erythematous base.
They are usually 3-10 mm in diameter and grow slowly, usually without signs or symptoms but occasionally they may become pruritic or tender. They may enlarge into broader, more elevated hyperkeratotic plaques several centimetres in diameter. Occasionally, a lesion grows to resemble an animal horn and is called a “cutaneous horn (often referred has hypertrophic AK).
Development of AKs may occur as early as the third or fourth decade of life in individuals who live in areas of high solar radiation, are fair-skinned with a history of extensive sun exposure, and do not use sunscreen for photoprotection. Usually, patients demonstrate a background of solar-damaged skin with telangiectasias, elastosis, and pigmented lentigines.
WHAT DOES AK MEAN?
The two words “actinic” and “keratoses” precisely describe what has happened to the skin.
“Actinic” comes from the Greek word for ray, “aktis,” and indicates that radiant energy (such as sunlight) has produced chemical changes.
The word “keratoses” means the skin has become hard and callous.
So AK literally means thickened scaly growth (keratosis) caused by sunlight (actinic).
WHAT DOES AK LOOK LIKE?
While AKs, usually multiple, share common characteristics, such as being flat to slightly raised or thickened, dry or crusty, scaly or warty, rough patch or bump on sun-damaged skin. But not all AKs look alike. Some are skin-colored and may be easier to feel than see. These lesions often feel much like sandpaper.
The base color may be light or dark, ranging from pink to red to brown, or a combination of these or the same color as skin.
Each one can range from the size of a pinhead to 2-3 cm across. The top of each one may have a yellow-white crust. They feel rough and dry, and are slightly raised from the surface of the skin.
Several solar keratoses may develop at about the same time, often in the same area of skin. Sometimes several join together and form a large flatish rough area of skin.
Solar keratoses usually develop on areas of skin which have been exposed to the sun a lot. For example, on the face, neck, bald patches on the scalp, and the backs of the hands. They may appear in other areas in people who do a lot of sunbathing.
There are usually no other symptoms. Rarely, may get an itchy, pricking or tender sensation from affected areas of skin. It can also become inflamed and surrounded by redness. In rare instances, actinic keratoses can bleed.
Aks later grow into a tough, wart-like area.
Sometimes AKs undergo rapid upward growth producing an exaggerated hyperkeratosis: a finger-like growth of hard skin, a horn-like projection above the skin surface appears to come out of a solar keratosis : it becomes a “cutaneous horn,” so named because it resembles the horn of an animal. The size of a cutaneous horn may range from that of a pinhead to a pencil eraser, and the shape may be straight or curved. Sometimes skin cancer hides below a cutaneous horn.
The skin around an AK tends to show evidence of sun damage, such as wrinkles and furrows (deep wrinkles).
Clinically AK can be divided in three grades:
-
Grade I - easy visible, slightly palpable (feels better than seen)
-
Grade II - easily visible, palpable (easily felt and seen)
-
Grade III - frankly visible, hyperkeratotic (clinically obvious)
The lesions begin as small, rough spots that are easier felt than seen with a sandpaperlike texture . With time, the lesions enlarge, usually becoming red and scaly. Most lesions are only 3-10 mm, but they may enlarge to several centimeters in size.
Actinic keratoses may show the following variants:
- Hyperkeratotic actinic keratosis(hornlike projection known as cutaneous horn)


- Bowenoid actinic keratosis

- Pigmented actinic keratosis (also known as spreading pigmented AK, displays a variable color, ranging from brown to yellowish-black, with a smooth, verrucous or slightly scaly surface)



- Lichenoid (lichen planus-like) actinic keratosis (a pink papule or plaque, frequently located on the upper extremities and upper torso, and may be difficult to differentiate clinically from BCC).

- Atrophic actinic keratosis(lacks the epidermal proliferation seen in the hypertrophic type)

Overlapping between subtypes may be observed.
WHO GETS ACTINIC KERATOSES?
Because long-term UV light exposure is implicated as the cause of Aks and AKs frequency correlates with cumulative UV exposure, AKs are more common in patients aged 50 years and older.
The typical patient with AKs is an elderly, fair-skinned, sun-sensitive person.
AKs occur almost exclusively in whites, especially those fair skin, redheaded or blond with blue, green or hazel eyes, who burn frequently and tan poorly. Because their skin has less protective pigment, they are the most susceptible to sunburn and other forms of sun damage.
According with Fitzpatrick skin type, patients with AKs tend to have Fitzpatrick type I or II skin, which burns and does not tan. The prevalence is reduced in persons with Fitzpatrick types III, IV, and V skin and is nonexistent in those with Fitzpatrick type VI skin. Sensitivity to UV light is inherited.
The incidence increases with each decade of life and is greater in residents of sunny countries closer to the equator. Men have a slightly increased frequency of AK.
But AKs also affect individuals with a history of cumulative sun exposure, who have had increased sun exposure and higher-intensity exposure such as having worked outdoors for long periods or who work with substances that contain polycyclic aromatic hydrocarbons such as coal or tar. For exemple roofers that work with tar and outdoors.
Sun-damaged skin is also dry, discoloured and wrinkled.
Patients immunosuppressed following organ transplantation are at markedly increased risk of developing AKs just like people affected by albinism or xeroderma pigmentosum, whose skin is very sensitive to UV rays.
WHEN DOES AK APPEAR?
As it usually takes years of sun exposure to develop an AK (because directly correlated to cumulative UV exposure), older people tend to be the most commonly affected. So likelihood of developing Ks increases with age, and lesions usually appears after age 50. But Aks may appear at a much earlier age in people who live in geographic areas with year-round high-intensity sunlight, who work outdoors, or who do a lot of sunbathing or use tanning beds and sun lamps.
Development of actinic keratoses may occur as early as the third or fourth decade of life in patients who live in areas of high solar radiation, are fair-skinned, and do not use sunscreen for photoprotection.
Summarizing, frequency increases with skin type, age (50 years and older), proximity to the equator, outdoor occupation, amount of sun damage.
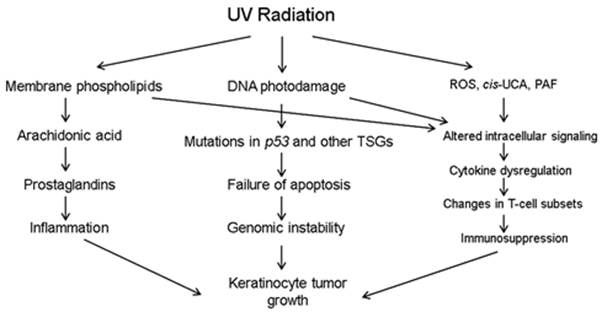
WHY DOES AK APPEAR?
Ak is a reflection of abnormal skin cell development due to exposure to chronic exposure to ultraviolet light (both UVB -290-320 nm and UVA -320-400 nm). While UV-A (320 - 400 nm) induced photo-oxidative stress indirectly induces characteristic DNA mutations, UV-B (290 - 320 nm) irradiation directly results in the formation of cyclobutane (thymin) dimer formation in DNA and RNA. If there are no appropriate repair mechanisms, these DNA changes are the starting phase of keratinocyte mutations which can progress into the development of AKs. UV radiations are not only the initiators but also the promoters. Other factors that can induce AKS are repeated iatrogenic exposure to UV-A, with or without combination with psoralenes, X-rays or radioisotopes.
The skin is normally pretty good at repairing any minor damage. Indeed overexposure to UV in normal skin induces an intrinsic, highly complex programme of auto-orchestrated cell death (p53-dependent apoptosis), which serves to protect the skin from damaged cells. Histologically these individual apoptotic keratinocytes are often seen in the epidermis of skin overexposed to sunlight or UV radiation and are known as "sunburn" cells.
But, over the years, some areas of skin are unable to cope with the repeated exposure to sun: UVs induce mutations of the tumor suppressor gene TP53 and basal keratinocytes with mutated TP53 may not respond normally to UV-induced apoptosis, allowing further proliferation and development of new genetic abnormalities.
Immunosuppression following solid organ transplantation may increase the risk for aktinic keratosis, but, only if there is sun exposure.
So, it is not a recent bout of sun-tanning that causes them but repeated minor sun-damage to the skin over time: AK frequency correlates with cumulative UV exposure.
Some of AKs may progress (risk from .025% to 16%) to invasive squamous cell carcinoma (SCC) with metastatic potential.


WHERE DOES AK APPEAR?
It may appear on any areas of the body that has been heavely exposed for years to sun exposure, such as the backs of hands, face, dorsal forearms, neck, nose, ears, cheeks, temples, forehead, bald scalp or lips.
However, it may occur on any area that is repeatedly exposed to the sun, such as the back, the chest, and the legs.
When such a lesion occurs on the lip the condition is called “actinic cheilitis” (“cheilitis” means inflammation of the lips).
Actinic cheilitis, commonly known as “sailor’s lips” or “farmer’s lips” is characterized by a diffuse scaling on the lower lip that cracks and dries. Sometimes the lip has a whitish discoloration on the thickened lip.
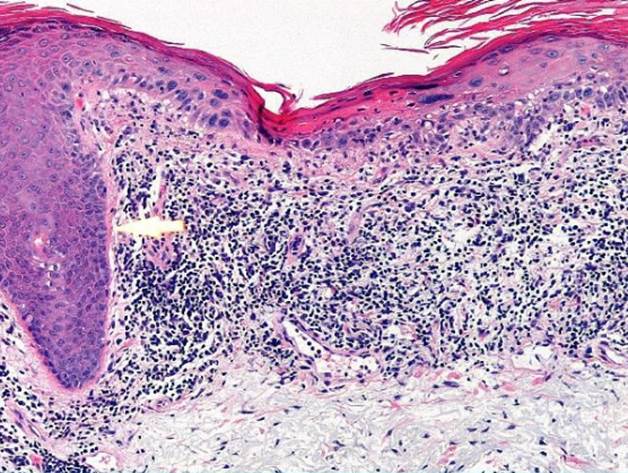
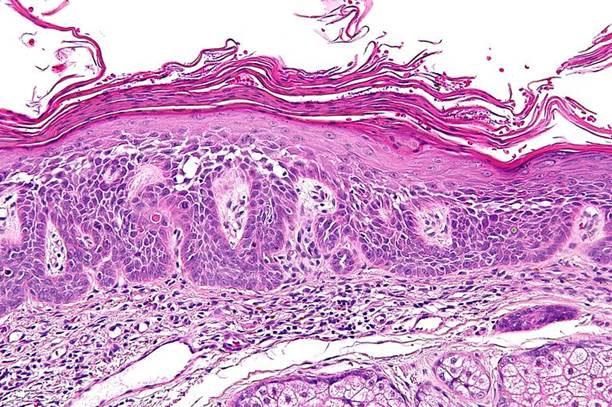
HISTOLOGIC FEATURES
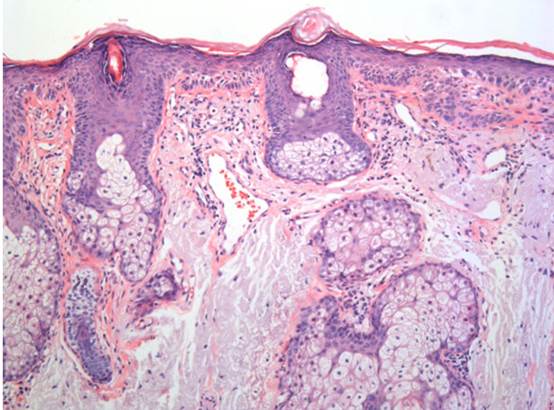
Actinic keratosis is characterized by dysplasia and architectural disorder of the epidermis, as follows:
- Abnormal keratinocytes of the basal layer that are variable in size and shape
- Altered cellular polarity (loss of polarity with a disorderly arrangement)
- Nuclear atypia
- Hyperkeratosis and parakeratosis (nucleated keratin layer) of the epidermis
- Irregular acanthosis may be present
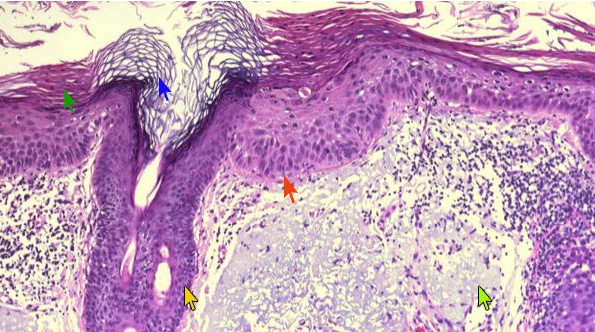
Histological diagnostic clues
Compact hyperkeratosis
Displastic basal cells
Actinic dermal changes
To remember that if there is no hyperkeratosis and no actinic dermal change, the lesion is not an actinic keratosis.
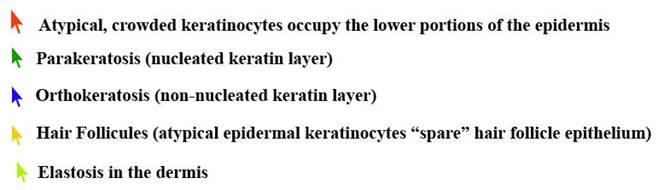
Buds of dysplastic epidermis may extend toward the papillary dermis. In some cases, these buds may be difficult to distinguish from superficially invasive squamous cell carcinoma, especially in a superficial shave biopsy.
The dysplastic epidermal changes typically spare the cutaneous appendages (hair follicles, sebaceous glands and apocrine and eccrine ducts). In contrast to the epidermal keratinocytes, the cells of the hair follicles and eccrina ducts that penetrate the epidermis within actinic keratoses retain their normal appearance and keratinize normally. Occasionally, cells of the normal adnexal epithelium extend over the atypical cells of the epidermis in an umbrella-like fashion.
There may be hyperpigmentation of the epidermis, trauma-related changes (ulceration, lichen simplex chronicus), as well as an inflammatory response.
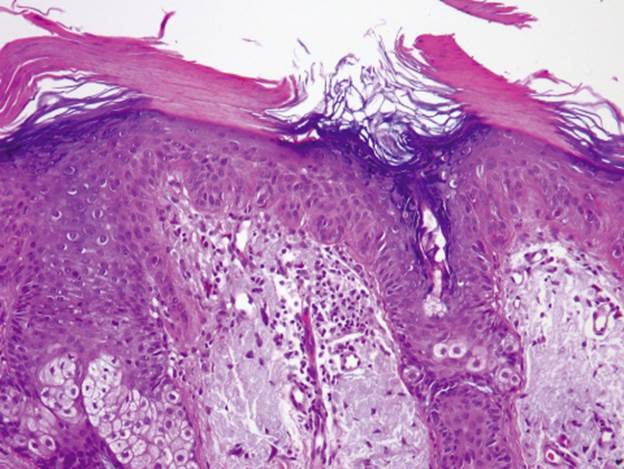
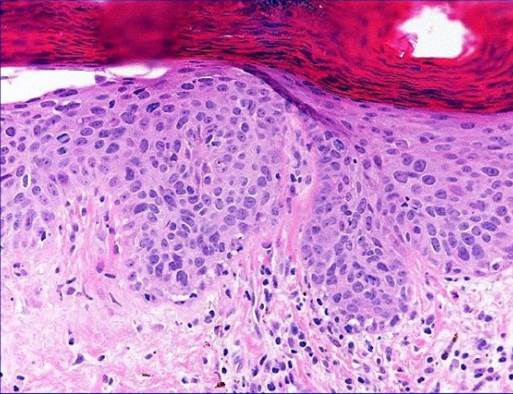
The primary histologic feature is atypia or dysplasia of the keratinocytes in the basal layers of the epidermis. This is often accompanied by parakeratosis, thinning of the granular layer, buds of atypical epidermis extending toward the papillary dermis, dermal solar elastosis, and inflammation.
The degree of intraepidermal involvement by keratinocytic atypia is graded as mild (AK I), moderate (AK II) or severe (AK III). In grade I the atypical keratinocytes are found in the basal and suprabasal layer, whereas in grade II atypical keratinocytes extend to the lower two-thirds of the epidermis, whereas in grade III full thickness atypia of the epidermis isfound, which is equivalent of changes previously called SCC in situ.
The epidermis shows mild hyperkeratosis with dysplasia of the basal keratinocytes and formation of small buds extending into the papillary dermis. There is prominent solar elastosis in the superficial dermis. The dysplastic changes primarily affect the epidermis between follicles.
The basal keratinocytes show dysplastic changes, including nuclear enlargement, hyperchromasia, increased cytoplasm, and form small buds that extend into the papillary dermis. There is subtle hyperkeratosis of the stratum corneum.
Variants or subtypes of actinic keratosis that have been described include:
- pigmented,
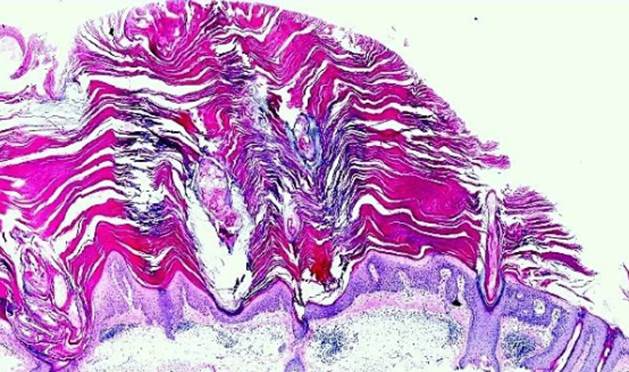
- hypertrophic,
- atrophic,
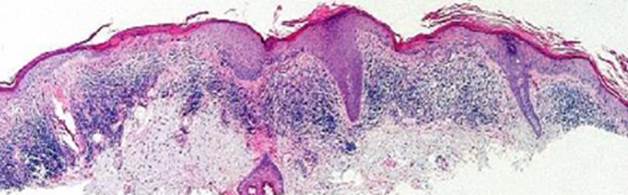
- lichenoid,
- acantholytic,
- Bowenoid.
Pigmented actinic keratosis, also known as spreading pigmented actinic keratosis, may show an increase in melanin pigment within basal layer keratinocytes and macrophages in the superficial dermis. Clinically and histologically this lesion may mimic a melanocytic proliferation. In such cases melanocytic markers (S100, Melan-A/Mart-1, MiTF, tyrosinase) may be useful to rule out a melanocytic lesion.
Hypertrophic actinic keratosis is common of the dorsal hand or forearm. Such lesions often show changes of lichen simplex chronicus due to chronic irritation and rubbing of the lesion.
Lichenoid actinic keratosis shows nuclear atypia, irregular acanthosis and hyperkeratosis and interface changes, including basal cell liquefaction, degeneration of the basal cell layer associated with a bandlike lymphocytic infiltrate within the superficial dermis in close apposition to the epidermis. Plasma cells may be present in the lichenoid infiltrate.
Acantholytic actinic keratosis may mimic other conditions associated with acantholysis, such as Grover disease, Darier disease. The degree of acantholysis can vary.
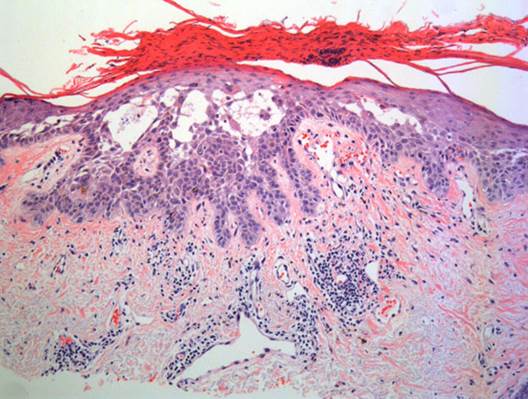
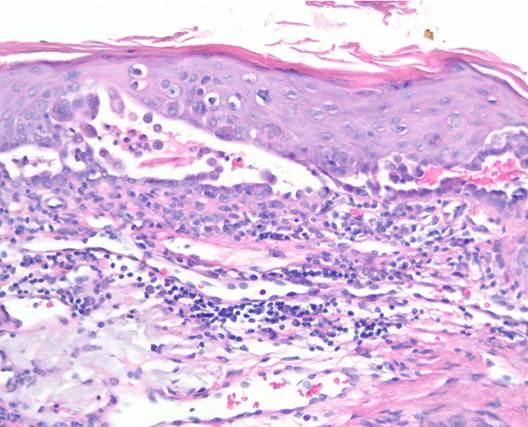
In theatrophic typeof actinic keratosis, hyperkeratosis usually is slight and the epidermis is thinned and devoid of rete ridges. Atypical cells with large hyperchromatic nuclei are found predominantly in the basal cell layer close together,. The atypical basal layer may proliferate into the dermis as buds and ductlike structures. It may also surround as cell mantles the upper portion of pilosebaceous follicles and sweat ducts, the epithelium of which otherwise appears normal.
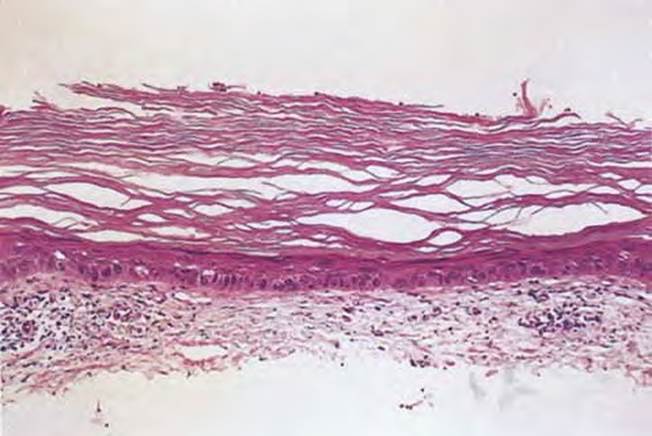
The bowenoid typeof actinic keratosis is histologically indistinguishable from Bowen's disease and may also be referred to as squamous cell carcinoma in situ. As in Bowen's disease, there are full thickness changes within the epidermis with considerable disorder in the arrangement of the nuclei, as well as clumping of nuclei and dyskeratosis.
Recapitulating:
The histopathological features of early lesions are:
- Focally atypical keratinocytes (large pleomorphic nuclei,
- hyperchromatic nuclei) in the basal layer of the epidermis
- Crowding of nuclei
- Neoplastic cells spare both acrosyringia and acrotrichia
- Alternation of ortho- and parakeratosis
- Actinic elastosis
of fully developed lesions:
- Hyperplasia (or sometimes atrophy) of the epidermis
- Rete ridges arranged in buds or columns
- Alternation of ortho- and parakeratosis
- Atypical epidermal keratinocytes involve mostly the lower half of the
- epidermis. Sometimes with focal involvement of the entire thickness
- of the epidermis
- Atypical keratinocytes extend along adnexal epithelia
- Dyskeratotic cells and mitotic figures
- Actinic elastosis
- Lymphocytic infiltrate of variable density
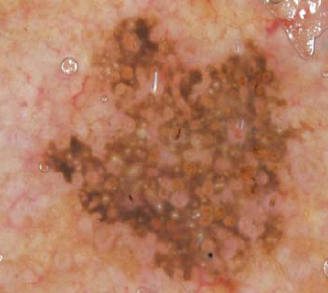
DERMOSCOPY
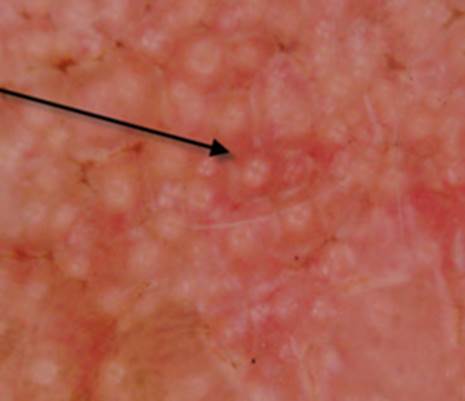
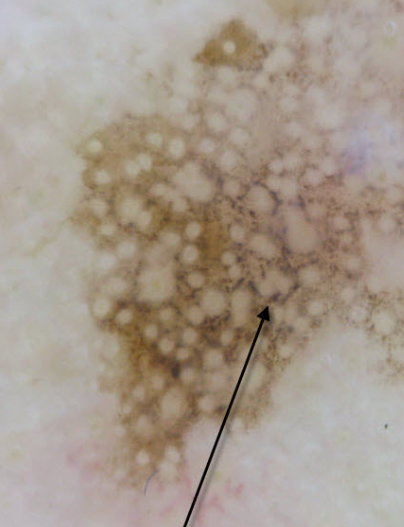
A typical feature of facial non-pigmented AK is a pattern named “strawberry-like pattern”, characterized by a background erythema/red pseudonetwork consisting of unfocused, large vessels located between the hair follicles, associated with prominent follicular openings surrounded by a white halo.

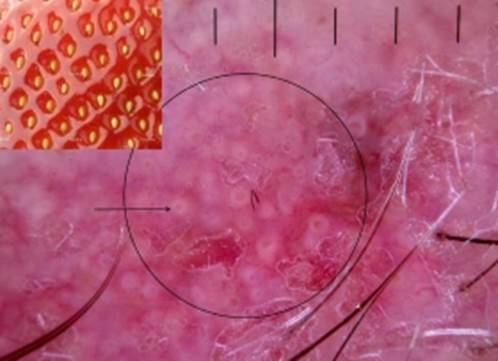
The arrow denotes one of the many 'pips'. These findings will only be evident in lesions with little scale, or where the scale has been lifted off.

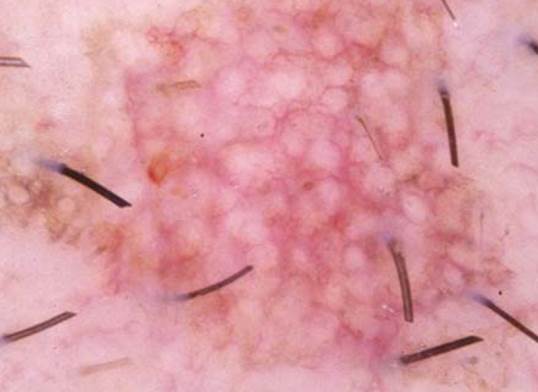
Strawberry appearance: white-to-yellow follicular keratotic plugs (circle) surrounded by a whitish halo encircled by wazy vessels. There is a background erythema/red pseudonetwork.
In AK located on the face and in hyperkeratotic AK, the yellowish keratotic plugs within the hair follicles have a targetoid appearance.
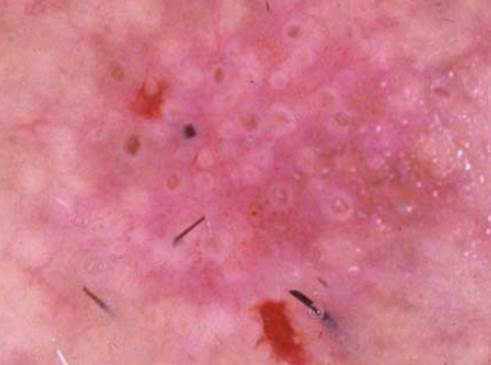
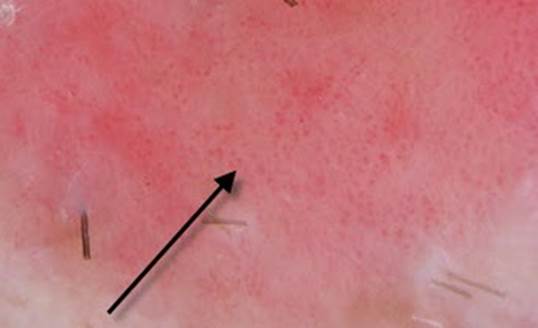
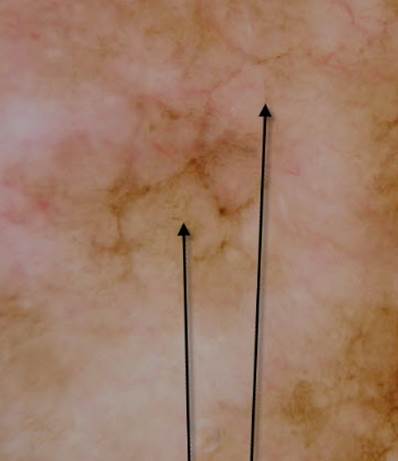
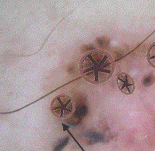
Inlfamed AK tend to have white circles on a pink background. The circles have 4 white dots in them called rosettes
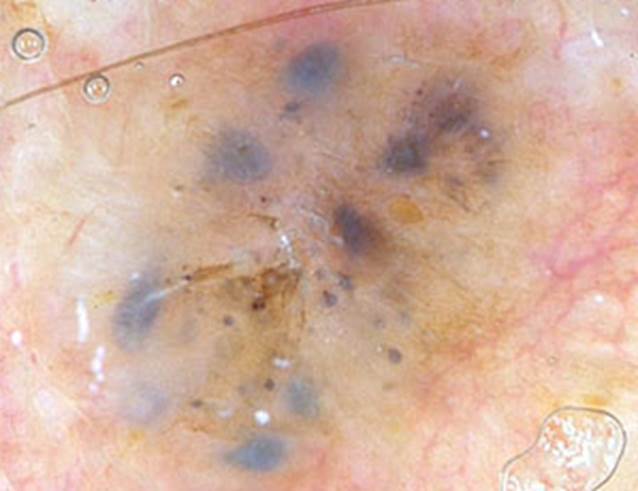
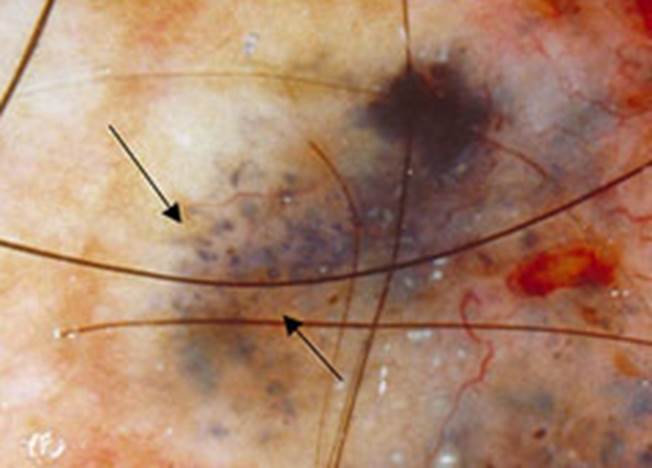
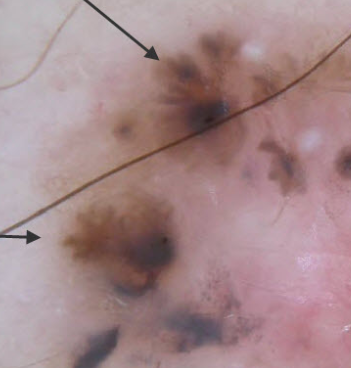
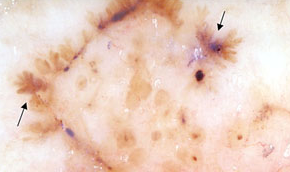
Dermoscopic characteristics of pigmented AK on the face include multiple slategray to dark-brown dots and globules around the follicular ostia basically uniform in size and regular in distribution. They correspond to aggregates of melanin-loaded macrophages located in the upper dermis.

Over time, the coalescence of small, gray to brown dots and globules around hair follicles gives rise to an annular-granular pattern.

A brown to gray pseudonetwork can be observed also in a high proportion of lesions.

In some cases, solar lentigo (lentigo senilis) on the face may clinically simulate pigmented AK. Dermoscopic features of solar lentigo include delicate light brown typical pseudonetwork and a regular diffuse pigmentation.
The presence of moth-eaten border at the periphery of the lesion and pigment appearing as smear (so-called jelly sign or jelly-like border)(the pigment appears on the skin surface such a jelly smear covering the skin)) is highly indicative of solar lentigo.

Dermoscopic analysis of the vascular pattern is indicated in differentiating non-pigmented AKs from teleangectatic rosacea and a variety of non-pigmented neoplasms, both nonmelanocytic and melanocytic. In facial non-pigmented AK a vascular pattern composed of linear wavy vessels or, less frequently, of small, coiled vessels and dotted vessels.
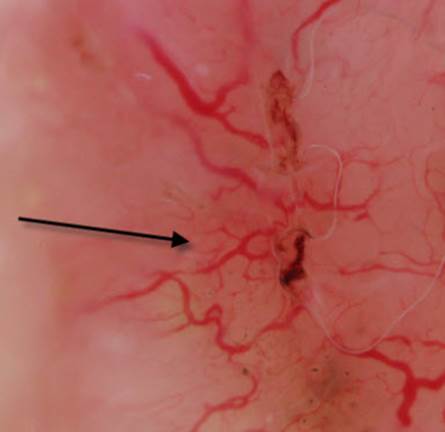
In teleagectatic rosacea the reddish pesudonetwork show a vascular plexus that consists of poligonal vessels

Squamous cell carcinoma (SCC) is characterized by pink coiled and dotted vessels

Non-pigmented basal cell carcinoma(BCC) shows pathognomonic serpentine vessels in branched pattern (arborizing telangiectasia consisting of vessels with different diameters and numerous branches).
Regular hairpin vessels are found in seborrheic keratosis

A vascular pattern characterized by glomerular vessels is present in non-pigmented Bowen’s disease
Dotted vessels arranged like pearls in a line are observed in clear cell acanthoma

Dotted vessels associated with linear irregular, polymorphous/ atypical and hairpin vessels, in the absence of a pigment network, are commonly found in amelanotic and hypomelanotic melanoma.

Dotted vessels associated with linear irregular, polymorphous/ atypical and hairpin vessels, in the absence of a pigment network, are commonly found in amelanotic and hypomelanotic melanoma.

In case of pigmented AK on the face, three are the differential diagnosis:
- lentigo maligna (LM) (the most important)
- pigmente basal cell carcinoma (BCC),
- pigmented seborrheic keratosis
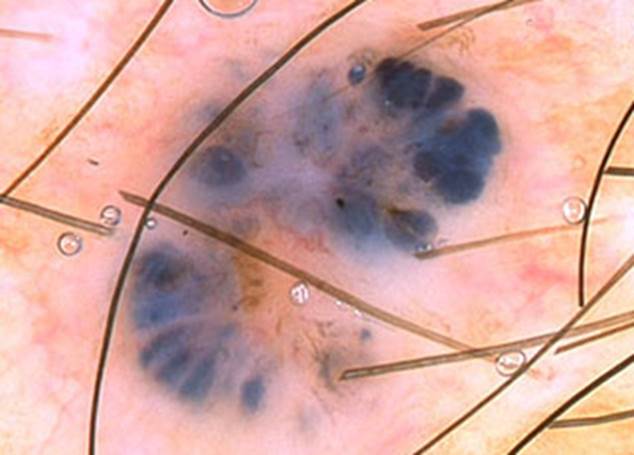
Lentigo maligna
Dermoscopically early phase of LM presents asymmetrically pigmented follicular openings (usually not found in pigmented AK).
Slatery dots and globules in LM are less uniform in size and and have less regular distribution than those found in AK.
Finally the absence of the rim of hyperpigmentation around follicular ostia allows to distinguish pigmented AK from LM. Grey perifullicolar circles made up of grey dots.
Other useful distinguishing feature of lentigo maligna are poligons
Pigmented BCC
Pigmented BCC may clinically simulate pigmented AK. Typical dermoscopic features of pigmented BCC immediately establish the diagnosis:
brownish-gray to gray-black leaf-like areas, usually located at the periphery of the tumor, are brown to gray-blue discrete bulbous extensions forming a leaf - like pattern. They should be distinguished from pseudopods because leaf areas are discrete pigment nests (islands) never arising from a pigment network and ususally not arising from an adjacent confluent pigmented area.
Large blue - gray ovoid nests are well circumscribed confluent or near confluent pigmented ovoid or elongated areas, larger than globules, and not intimately connected to a pigmented tumor body
Multiple blue-gray globules are well circumscribed confluent or near confluent pigmented ovoid or elongated areas, larger than globules, and not intimately connected to a pigmented tumor body
Spoke wheel areas are well circumscribed radial projections, usually tan in color but sometimes blue or gray, meeting at an often darker (dark brown, black or blue) central axis.
Pigmented seborrheic keratosis on the face
Pigmented seborrheic keratosis on the face is distinguished by a typical pigmented pseudonetwork with regular meshes and holes, opaque areas, pseudofollicular openings and horny pseudocysts.
DOES AK UPGRADE IN A SKIN CANCER?
Ak can be considered a disease continuum caused from Uv:
Photodamage skin – early AK – AK - SCC
So AKs are considered the earliest stage in the development of skin cancer and can give rise, in a small percentage of people with normally functioning immune systems, to a type of skin cancer called squamous cell carcinoma (SCC). This type of cancer usually isn't life-threatening if detected and treated early, but can be fatal because can grow and invade surrounding tissues, some spreading (metastasizing) to other parts of the body.
The risk of squamous cell carcinoma occurring in a patient with more than ten solar keratoses is about 10 to 15%.
In 98% to 99% of excised SCC, in the histology it’s possible to see AKs in the surrounding areas. So it is a disease continuum from normal skin to AK to invasive SCC.
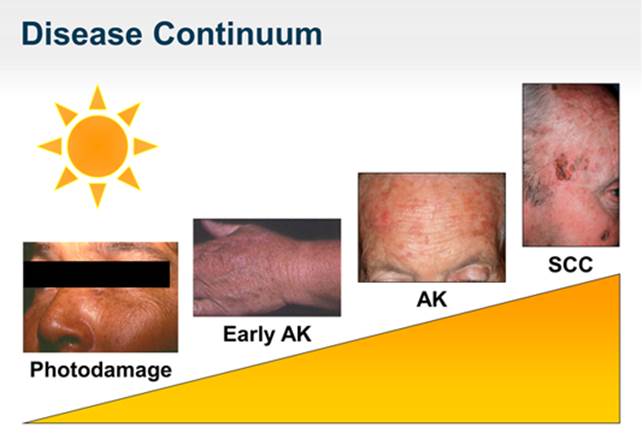
So the more keratoses people have, the greater the chance of developing skin cancer.
However, if treated early, almost all actinic keratoses can be eliminated.
Other factors that increase the risk of an AK progressing to SCC include
- advancing age,
- taking a medication or having a medical condition that suppresses the immune system (weak immune system),
- a personal or family history of skin cancer,
- fairer, less-pigmented skin
- skin sign of severe sun damage.
Signs of sun damage, also known as photodamage, include
- age spots,
- spider veins on the face (teleangiectasias),
- rough and leathery skin (elastosis),
- fine wrinkles that disappear when stretched,
- loose skin,
- pigmented lentigines
- blotchy complexion.
AKs may remain unchanged for years, but if an AK becomes thickened or ulcerated must get checked because it may have become a SCC.
DIFFERENTIAL DIAGNOSIS
- Arsenical Keratosis
- Basal Cell Carcinoma
- Benign Lichenoid Keratosis
- Bowen Disease
- Squamous Cell Carcinoma
- Superficial Basal Cell Carcinoma
- Discoid lupus erythematosus
- Seborrheic keratosis
- Warts, non genital
- Porokeratosis
- Lentigo
- Lentigo maligna
- Pigmented basal cell carcinoma
RISK FACTORS
Although anyone can develop actinic keratoses, pepole more likely to develop the condition are:
-
40 years of age or older
-
live in a sunny climate
-
live in geographic areas that receives year-round high-intensity sunlight,
-
have had periods of intense exposure to the sun
-
spend a lot of time outdoors in the summer
-
use tanning beds and sun lamps
-
spend a lot of time outdoors in the summer
-
live in an area that receives high-intensity sun year round (such as Florida or Southern California)
-
have a history of frequent or intense sun exposure or sunburn
-
have pale white to creamy white skin
-
have pale skin, especially when coupled with blue, hazel or green eyes
-
have blond or red hair
-
have blue, hazel, or green eyes
-
have a tendency to freckle or burn when exposed to sunlight
-
tend to freckle or burn when exposed to sunlight
-
have a personal history of an actinic keratosis or skin cancer
-
have a weak immune system as a result of chemotherapy, chronic leukemia, AIDS or as a conseguence of medication to prevent organ rejection long-term exposure to sunlight
-
receive chronic and intense sun exposure either through an occupation or leisure activity (e.g. farming, construction work, fishing, golfing and gardening)
WHEN TO SEE A DOCTOR
Because it can be difficult to distinguish between noncancerous spots and cancerous ones, if a spot or lesion
-
persists
-
is painful
-
itches or burns
-
oozes or bleeds
-
becomes scaly or crusty
-
grows
TREATMENT
Medical management of AK begins with educating and instructing the patient to limit sun exposure and to practice sun protection.
Photoprotection can be defined as “the use of physical and/or chemical agents to prevent the skin-damaging effects from UV radiation in sunlight.” Photoprotection should be applied year around, not only in hot sunny summer days.
Without it, the risk of developing new and recurrent AKs increases significantly.
Physical photoprotection is provided by clothing, umbrellas, parasols, awnings, trees, and tents.
Sunscreens provide chemical photoprotection.
Before heading outdoors, either to work or for a day of fun, sun protection is vital for all fair skinned people working or enjoying themselves outdoors.
Sun protection includes:
- wearing protective clothing, such as a wide-brimmed hat, long pants, and long sleeves;
- limitation of recreational exposure. Those who work outdoors should consider making adjustments in their work-related sun exposure.
- Application of a broad-spectrum sunscreen with a sun protection factor (SPF) 30 or more to all skin that will be exposed to the sun. “Broad- spectrum” means that the sunscreen contains ingredients that protect the skin from the sun’s UVA rays and UVB rays. UVA rays penetrate the skin more deeply than UVB rays and are the rays that contribute to premature aging and wrinkles. The UVB rays, also known as the burning rays, cause sunburn. Both UVA and UVB rays have been linked to the development of skin cancer. Sun protection should be practiced year round. While UV radiation is most intense during the summer months, more than 50% of UV radiation reaches the skin during the remaining months of the year when we usually do not think about sun protection.
- seeking shade.
- avoiding deliberate tanning.
Of course, staying out of the sun completely is the most effective way to protect their skin from the damaging effects of the sun’s ultraviolet (UV) rays.
But it’s never too late to begin protecting the skin from the sun’s harmful UV rays: it can be beneficial even if Aks are present because the development of these lesions is directly proportional to sun exposure and sun protection can prevent further damage allowing the body to repair some of the existing damage.
Patients should be cautioned to avoid sun exposure from 10:00 AM to 3:00 PM as much as possible.
About treatment, dermatologists consider a number of factors before choosing the most appropriate treatment method. Factors include:
-
Size, number, location, and stage of the lesions
-
Age, health, and medical history
-
Occupation
-
Cosmetic expectations and treatment preferences
-
Patient compliance (i.e., willingness to self-treat as needed for several weeks)
-
History of previous treatment
Treatment of a solar keratosis requires removal of the defective skin cells. New skin then forms from deeper cells which have escaped sun damage.
The procedures have various advantages and disadvantages, including
-
side effects,
-
risk of scarring,
-
the number of treatment sessions required.
It is not practical to remove all keratoses in those with very extensive sun damage; in such cases it is important to get rid of thickened or tender lesions as these are the ones at greatest risk of progressing to skin cancer.
Afterward it is important to have regular follow-up visits to check for new patches or lesions.
Treatment consists of 2 broad categories:
-
medical therapy.
-
surgical destruction of the lesion.
Medical therapy has the advantage of being able to treat large areas with many lesions. The possible disadvantages of medical therapies include lengthy courses of treatment with irritation and discomfort.
The medications are:
- topical 5-fluorouracil (5-FU, Efudix 5% cream) 5-FU is a topical chemotherapeutic agent (antimetabolite) that destroys clinical foci via interference with DNA and RNA by blocking the methylation reaction of deoxyuridylic acid to thymidylic acid. The lack of DNA synthesis, particularly in fast-growing dysplastic cells, prevents cell proliferation and causes cell death. It’s most useful when there are many keratoses on the face.The cream is applied onto facial skin once or twice daily for two to four weeks. The treated areas become red, inflamed, raw and cause discomfort. This treatment can be temporarily disfiguring, because of erythematous ulcerations and crust formation. Healing starts when the cream is discontinued: the lesions usually heal within 2 weeks of stopping treatment, the complexion is smooth and the eventual result is usually excellent.
- 5% imiquimod cream (Aldara), a member of the class of immune response modifier (immune enhancing agent), is a toll-like receptor 7 (TLR7) that stimulates the immune response by induction, sinthesis and release of a variety of cytokines, which, in turn, invoke a nonspecific anti-AK immune response (interferons, natural killer cells) and a specific immune response (cytotoxic T cells. It is applied to areas affected by solar keratosis (not larger than about 2 inches by 2 inches) once a day three times a week, (e.g. Monday, Wednesday, Friday) for four weeks. Imiquimod cream should be left on the skin for approximately 8 hours, no more than 1 packet to defined area of face or scalp to dry skin (at least 10 min after washing face) and leaving on for approximately 8 h; then, the area must be washed with mild soap and water. Aldara causes an inflammatory reaction, which is maximal at about three weeks and then gradually settles down with continued use. The results are variable, but generally excellent. Reaction to the drug is idiosyncratic, with some patients barely reacting and others developing marked inflammation. During treatment patients should
-
avoid exposure to sunlight or artificial tanning devices;
-
have regular use of sunscreen;
-
avoid contact with lips, eyes, or nostrils.
Common adverse effects include erythema, edema, vesicles, erosion or ulceration, weeping, exudate, flaking, scaling, dryness, and scabbing, or crusting. Subclinical lesions previously not appreciated may become inflamed during therapy. In patients with a brisk inflammatory response, dosing is reduced to twice or even once a week, with preservation of therapeutic efficacy but increased tolerability. Experimental evidence suggests patients may develop T-cell memory after treatment with this drug and thus may be less likely to develop new AKs in the future. Response rates show complete remission in 84%; a recurrence rate of 10% within 1-yearfollow up and 20% within 2-years follow up.
- topical diclofenac 3% gel, is a nonsteroidal anti-inflammatory drug that inhibits cyclooxygenase 2 and thus the upregulation of the arachidonic acid cascade and the production of prostaglandins. Prostaglandin E2 suppresses the production of immune-regulatory lymphocytes, T-and B-cell. Recommended duration of therapy is 60 to 90 days.
- photodynamic therapy (PDT) with topical delta-aminolevulinic acid. Topical photodynamic therapy (PDT) acts through the selective destruction of atypical keratinocytes (depth of penetration 3-4 mm) through light activation of a photosensitiser (a light-sensitizing compound) (a porphyrin chemical, delta-aminolevulinic acid) applied to the affected area prior to exposing it to a strong source of an appropriate wavelength visible light, in the presence of oxygen. Delta-aminolevulinic acid is a component of the heme biosynthetic pathway that accumulates preferentially in dysplastic cells than normal cells. Once inside these cells, it is enzymatically converted to protoporphyrin IX, a potent photosensitizer. The photosensitiser generates oxygen free radicals upon illumination, which results in selective photochemical and photothermal effects on the irradiated tissue and cell death results. The treated area become erythematous and crusted and then heals over a couple of weeks or so. Patients experience pain in the areas treated.
- Ingenol mebutate is a product derived from the Euphorbia peplus plant cultivated in Queensland, Australia. It is a gel available in two different concentrations: for treatment of the face and scalp the gel is applied at a concentration of 0.015% once daily for three consecutive days, whereas for treatment of the trunk and extremities the gel is applied once daily for two consecutive days at a concentration of 0.05%. After spreading evenly over the treatment area, the gel should be allowed to dry for 15 minutes. Patients should wash their hands immediately after applying the gel and take care not to transfer the applied drug to other areas, including the eye. Patients should avoid washing and touching the treated area, or participating in activities that cause excessive sweating, for 6 hours after treatment. Following this time, patients may wash the area with a mild soap. Hypertrophic and hyperkeratotic lesions were excluded from treatment. The most common local skin reactions are local skin reactions (erythema, flaking/scaling, vesiculation/postulation, crusting and swelling), application site pain, application site pruritus, application site irritation, application site infection, periorbital edema, nasopharyngitis and headache.
- Cryotherapy
- Curretage and cautery
- Excision biopsy
Cryotherapy is an effective treatment for single AKs. It uses a cryogen to lower the temperature of the skin and produces cell death. The most common cryogen used is liquid nitrogen, with a temperature of -195.8°C. The cure rates from 67 – 99%.
Other structures in the skin, such as collagen, blood vessels, and nerves, are more resistant to the lethal effects of cold than keratinocytes.
Thicker keratosis may be treated with curettage (curettage is the removal of a lesion by scraping it with a sharp instrument, providing a sample for histologic evaluation. This treatment requires local anesthesia.
Cautery or diathermy burns the keratoses off and prevents bleeding.
If lesions are nodular, indurated, unresponsive, or aresuggestive of invasive cancer to rule out an invasive squamous cell carcinoma, excision biopsy makes sure the lesion has been completely removed.
Other procedures:
resurfacing procedures, in which the entire epidermis is removed, sometimes with some portion of the dermis, are effective for AK eradication.
Resurfacing procedures include:
-
medium and deep chemical peels,
-
dermabrasion,
-
ablative laser resurfacing.
PROGNOSIS
The prognosis is good. With continuing surveillance and treatment, AKs can be managed individually.
However, the prognosis in a person with long-term exposure is more guarded because of the multitude of their lesions and the likelihood that some lesions may progress and develop into invasive squamous cell carcinomas.
PATIENT EDUCATION
To reduce the risk of developping AKs, it’s important to encourage patients
-
to wear sunscreens,
-
to limit sun exposure, , avoiding the sun between 10 a.m. and 4 p.m. when the sun's rays are the strongest, and not using tanning beds and sun lamps.
-
to adjust their hobby or profession to decrease sun exposure
People at risk should see a dermatologist regularly. The dermatologist should instruct how to perform a self-examination, to detect as early as possible:
-
a new lesion
-
a change to an existing lesion. A lesion is “changing” if the size or appearance changes or the lesion bleeds or itches.
PHOTOPROTECTION
Actinic keratoses (AKs) develop in skin that has been exposed to the ultraviolet (UV) light of the sun for years. Therefore, the best defense against AKs is to practice sun protection.
Sun-protection practices can prevent:
- AKs from developing
- New AKs from forming
- AKs from recurring (AKs sometimes return after treatment)
Ideally, sun protection should begin early in life because overexposure to UV radiation increases one’s risk of developing AKs. What many people do not realize is that sun protection can be beneficial at any age, even when signs of sun damage, such as AKs, have already appeared. Sun protection can prevent further damage. Research also shows that the skin’s recuperative powers can repair some of the damage when protected from ultraviolet (UV) light.
Photoprotection should be part of this comprehensive sun-protection plan. Everyone should remember, before to head outdoors, either to work or for a day of fun, to think photoprotection.
HOW:
-
wearing clothing that is dark colored and has a tight weave,
-
seeking shade whenever possible,
-
applying a broad-spectrum sunscreen that has an SPF of 30 or more to all exposed skin.
-
avoiding deliberate tanning from the sun and tanning beds
IN DETAILS
-
Select clothing for its photoprotection properties. Clothing with a high Sun Protection Factor (SPF) can block nearly 98% of UVA and UVB radiation. What gives clothing a high SPF is the fabric. Tightly woven synthetic fabrics made from nylon or polyester provide maximum photoprotection. The tighter the weave, the more sun protection provided. Almost as photoprotective, tightly woven cotton blends are more comfortable in hot and humid conditions. Conversely, light-colored fabrics with a loose weave, such as a white cotton t-shirt, do not provide adequate photoprotection - especially when wet. To get maximum photoprotection select dark colored, tightly woven clothing that covers the skin. Long sleeves and pants are preferable.
If you will be wearing a garment outdoors frequently, you may want to ask your dermatologist about companies that specialize in photoprotective clothing. Your dermatologist also may recommend a laundry additive that can increase the photoprotection provided by clothing.
Since clothing plays such an important role in photoprotection, some garments made specifically for outdoor activities, such as hiking, print the garment’s SPF on a highly visible tag. Fabrics used to make these clothes are woven specifically to provide UV protection and are made to meet SPF specifications.
-
Seek shade whenever possible. In addition to wearing protective clothing, the American Academy of Dermatology recommends that people seek shade whenever possible. Tents, trees, awnings, and manmade shade structures all provide photoprotection. Erecting a temporary open-air tent or permanent shade structure can provide effective shade and ultraviolet radiation protection for an outdoor area. Whenever possible, seek a shady place.
-
To be effective, a sunscreen must be:
-
Broad-spectrum and have an SPF or 30 or more
-
Used on a regular basis, including cloudy days since 80% of the sun’s UV rays pass through the clouds
-
Applied to dry skin 15-30 minutes before going outdoors, reapplied after 20 minutes and then approximately every two hours to all exposed skin
-
Applied to all bare skin - a lip balm that contains sunscreen with an SPF 30 or higher protects the lips
-
Reapplied after perspiring or swimming
-
Wear a wide-brimmed hat with a brim that circles the entire hat and shades your face and neck from the sun’s rays.
-
Use extra caution near water, snow, and sand. These reflect the damaging rays of the sun, which can increase your chance of sunburn.
Aside from AKs, the sun’s UV rays also cause:
-
Premature aging (mottled skin, loss of skin’s firmness)
-
Immunosoppression that weaks the body’s ability to protect itself from cancer and other diseases)
-
Cataracts and macular degeneration (leading cause of blindness in people aged 65 and older)
WHAT TO KNOW ABOUT SUNSCREEN?
Sunscreen provides photoprotection for exposed skin.
The American Academy of Dermatology recommends that anyone who will be in the sun for 20 minutes or more wear a broad spectrum (offers protection from both UVA and UVB rays) sunscreen with an SPF of at least 15 on all exposed skin year-round. Sunscreens are designed to aid the body’s natural defense mechanisms in protecting against harmful ultraviolet (UV) radiation from the sun. They work by absorbing, reflecting, or scattering the sun’s rays on the skin. Since some UV light gets through sunscreens, they should not be the only means of protecting the skin from the sun’s UV rays.
Sunscreen should not be used to prolong sun exposure or only to avoid sunburn.
Sunscreen does not make sunbathing safe.
To be effective, a sunscreen must be:
-
High-quality sunscreen
-
Broad-spectrum and have an SPF or 15 or more (broad-spectrum protects against both UVA and UVB rays).
-
Used on a regular basis, including cloudy days since 80% of the sun’s UV rays pass through the clouds
-
Applied generously to dry skin at least 30 minutes before going out into the sun, and reapplied frequently (every two hours to all exposed skin).
-
enough (one ounce) to fill a shot glass (29.57 ml), to cover the exposed areas of the body properly.
-
used year-round, even on cloudy days, including in the winter.
-
applied to all exposed skin –
-
applied to the lip with a lip balm that contains sunscreen with an SPF 15 or higher.
-
Applied on the ears, neck, and hands.
-
Reapplied every two hours
-
Reapplied after perspiring, strenuous activity or swimming.
Sunscreen comes in many forms (e.g. creams, gels, lotions, wax sticks). The type of sunscreen used is a matter of personal preference.
The use of sunscreen is not limited to warm and sunny areas: The risk for AKs can be substantial in far northern latitudes, especially when a person has AK risk factors such as white skin, red or blond hair, a tendency to freckle or burn when exposed to sunlight, and blue, green, or gray eyes.
PREVENTION
Solar keratoses may be prevented by protecting skin from ultraviolet radiation. If already present, keratoses may even improve with regular application of broad spectrum sunscreen to affected areas every day. Sun protection is vital for all fair skinned people working or enjoying themselves outdoors.
If you spend much time in the sun you have an increased risk of developing solar keratoses.
Preventive measures recommended for AK are similar to those for skin cancer:
- Avoiding sun for long periods of time without protection (e.g., sunscreen,clothing, hats).
- Limiting the time in the sun. Avoid staying in the sun so long that you get a sunburn or a suntan. Sun exposure accumulated over time cause actinic keratosis. Set time limits when at the pool or beach or when you're spending time outdoors in the winter. Snow, water and ice all reflect and intensify the sun's harmful rays, and ultraviolet rays are strongest between 10 a.m. and 4 p.m. Clouds block only a small portion of UV rays.
- Applying frequently and generously powerful sunscreens with SPF ratings greater than 30 and that also block both UVA and UVB light.
- Covering up when you must be in the sun wearing sun protective clothing such as wide-brimmed hats, long-sleeved shirts, long skirts, or trousers and sunglasses that protect against both UVA and UVB rays.
- Avoiding sun exposure during noon hours, between 11 am and 3 pm (ultraviolet light is the most powerful at that time).
- Avoiding deliberate tanning (from the sun and tanning beds). If you want to look like you’ve been in the sun, consider using a sunless self-tanning product.
- Using extra caution near water, snow, and sand. These reflect the damaging rays of the sun, which can increase your chance of sunburn.
- seeking natural shade in the form of trees or other shelter
- Avoiding tanning beds and tan-accelerating agents. Tanning beds emit UVA rays, which are often touted as less dangerous than UVB rays. But UVA light penetrates deeper into your skin, causes actinic keratosis and increases your risk of skin cancer. Also, avoid using suntan-accelerating products. Bronzing lotions that produce a tanned look without any sun exposure are a safe choice as long as you continue to use sunscreen outdoors.
- Covering up. For extra protection from the sun, wear tightly woven clothing that covers your arms and legs and a broad-brimmed hat, which provides more protection than does a baseball cap or golf visor. You might also consider wearing clothing or outdoor gear specially designed to provide sun protection.
- Being aware of sun-sensitizing medications. Some common prescription and over-the-counter drugs can make your skin more sensitive to sunlight. These include antibiotics; certain cholesterol, high blood pressure and diabetes medications; birth control pills; nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin, others); and the acne medicine isotretinoin (Accutane). Ask your doctor or pharmacist about the side effects of any medications you take. If they increase your sensitivity to sunlight, be sure to take extra precautions.
- Checking the skin regularly and reporting changes to the doctor. Examine your skin regularly, looking for the development of new skin growths or changes in existing moles, freckles, bumps and birthmarks. With the help of mirrors, check your face, neck, ears and scalp. Examine the tops and undersides of your arms and hands.
- Using sunscreen. Before spending time outdoors, apply a broad-spectrum sunscreen with a sun protection factor (SPF) of at least 15. Some sunscreens contain substances that block ultraviolet A (UVA) as well as ultraviolet B (UVB) rays. UVA rays penetrate into the deeper layers of your skin and can weaken your skin's immune system; UVB rays cause sunburn and play a significant role in superficial skin cancers. Using sunscreen on all exposed skin, including your lips. Apply sunscreen 30 minutes before sun exposure and reapply it every few hours or more often if you swim or sweat. Apply sunscreen to infants or young children before going outdoors and teach older children and teens how to use sunscreen to protect themselves. Keep a bottle of sunscreen in your car, your boat, with your gardening tools, and with your sports and camping gear to remind yourself and your family to use it.

