ERYTHROMELALGIA
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it

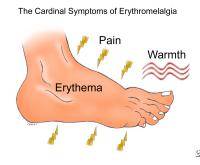
Erythromelalgia is a rare condition characterized by episodes of intense burning pain, erythema (marked redness) and warmth (increased skin temperature), primarily of the feet and hands.
It is also known as Mitchell’s disease (from Silas Weir Mitchell, an American physician who reported the first case in 1878), acromelalgia, red neuralgia, erythermalgia. This last term was proposed by Smith and Allen to emphasize the characteristic warmth.
The name derives from 3 Greek words:
-
erythros(“red”)
-
melos (“limb”)
-
algos (“pain”)
The condition is classified and differentiated into two types:
-
primary erythromelalgia
-
secondary erythromelalgia
Primary erythromelalgia (autosomal dominant mode of inheritance), develops spontaneously without any associated underlying disease. It results from genetic mutation.
In this condition there are mutations (abnormal changes) in the gene that codes for a specific sodium channel (which is present in nerves and is responsible for pain transmission). It is believed to arise in the SCN9A gene that provides instructions for making one part of a sodium channel called NaV1.7. The NaV1.7 sodium channels are found in specific nerve cells called nociceptors, neurons located just outside the spinal cord, which are involved in trasmitting pain signals (sensation and conduction of pain stimuli).
Sodium channel transport positively charged sodium atoms (sodium ions) into cells and play a key role in a cell’s ability to generate and transmit electrical signals. The mutations in the SCN9A gene result in a NaV1.7 sodium channel that opens more easily than normal and stays open for a greater duration than in usual cases, enhancing the trasmission of pain signals (because of the increase in sodium ions flow into nociceptors)) and leading to the appearance of the signs and symptoms of the disease.
Patients affected by primary erythromelalgia are normally young (before 25 years old) when the symptoms start, with a male to female ratio being 1:2.5.
Attacks can last from an hour to months at a time and occur infrequently to frequently with multo
Secondary erythromelalgia develops as a result of other disorders, most commonly:
-
Neurological diseases (e.g. multiple sclerosis, peripheral neuropathy)
-
Autoimmune diseases (e.g. LES, diabetes mellitus)
-
Mieloproliferative disorders ( the blood-producing cells in the bone marrow develop and reproduce abnormally)(e.g. polycythaemia vera -increased red cells-, essential thrombocythaemia -increased platelets-). In this cases erythromelalgia presents before the appearance of mieloproliferative disorders in 85% of cases.
-
Medicinal side effects (nifedipine, felodipine, nicardipine bromocriptine, topica isoprapanol, verapamil, pergolide-withdrawn from US market on 2007)
-
Mushromms ingestion (two species of related fungi, Clitocybe acromelalga from Japan and Clitocybe amoenolens from France, has led to several cases, which lasted from 8 days to 5 months)
The discomforting episodes of this syndrome are usually triggered by an increase in body temperature, such as:
-
from workouts, wearing tight socks or shoes for too long,
-
staying in warm environs (temperature over 84°F-29°C) for a prolonged duration,
-
ingestion of spicy foods,
-
ingestion of alcohol,
-
caffeine consumption,
-
over-exertion or exercise
and any pressure applied to the limbs. In some patients sugar and even melon consumption have also been known to provoke attacks.
However symptoms can also flare-up without any external stimulation.
The condition usually involve the lower extremities (soles of the feet and toes) but fingers and hands can be involved. Involvement is usually bilateral (both feet and/or hands), though not necessarily symmetric. Less frequently, symptoms may appear in the face.
The classic description of erythromelalgia is a triad of red, painful and warm feet or hands, brought on the warming and relieved by cooling. The intensity of symptoms can vary from one patient to another. Some individuals experience moderate tingling sensation which persist for only a few minutes. Others suffer from acute pain. Some patients notice a continual burning while others only flare-up that may last minutes to days and tipically occurs late in the day and continue through the night. Usually episodes begin with an itching sensation progressing to a more severe pain with a burning sensation.
Pain may be so intense that normal functioning and quality of life are greatly affected. Some patients become virtually housebound by the continuous flare-ups and pain: they cannot wear socks or closed shoes, even in winter. Daily activities such as walking and wearing shoes are impossible.
There are not specific diagnostic tests to detect erythromelalgia. The initial diagnosis of the disorder is based on the signs reported by the patient as well as on the clinical picture of the feet and hands, sometimes difficult because of the intermittent nature of the disease. It is important to look for symptoms of any underlying condition: e.g. erythromelalgia may be an early, preceding sign of a mieloproliferative disorder (by 2.5 years). If no known underlying cause has been found, the erythromelalgia is considered primary.
Treatment of the symptoms of both primary and secondary erythromelalgia is primarily medical and supportive and is through
-
general non medical measures
-
drug therapy
-
surgical intervention
1. General non medical measures
Cooling and elevating the extremities may temporary relieve symptoms. Care is needed around cold water immersions because frequent immersion can:
-
create a vicious cycle as the changes in temperature may cause reactive flaring,
-
lead to maceration of the skin, non-healing ulcers, infection, gangrene and amputation.
Patients should avoid excessive warming or dependency of the extremity as vigorous exercise.
2. Drug therapy
-
Capsaicin cream, with varying results
-
A variety of oral medications have been used to relieve symptoms, including:
-
Aspirin – promptly relieves symptoms of erythromelalgia involving myeloproliferative disorders. Aspirin inhibits prostaglandin synthesis, which prevents formation of paltelet-aggregating thomboxane A2.
-
Anagrelide- in cases secondary to myeloproliferative disorders. It inhibit cyclic nucleotide phosphodiesterase and the relase of arachidonic acid from phospholipase. A decrease in megakaryoryte hypermaturation may result in a reduction in platelet production.
-
Serotonin re-uptake inhibitors – venlafaxine, sertraline, fluoxetine, paroxetine
-
Tricyclic antidepressants –amitriptyline, imipramine
-
Anticonvulsants –gabapentin
-
Lidocaine plus mexiletine(affect voltage-gate sodium channels)
-
Prostaglandins – misoprostol
-
Intravenous infusions of nitroprusside, lidocaine and prostaglandin
3. Surgical intervention
Surgical sympathectomy (a procedure in which the sympathetic nerve fibres are selectively cut) has be attempted with variable results. Patients respond quite variably to drug therapy and no single therapy has proved consistently effective. Spontaneous remissions have also been known to occur. The differential diagnosis of erythromelalgia is from disorders that produce similar symptoms. These include:
-
Complex regional pain syndrome (CRPS), presents with severe burning pain and redness . Symptoms are often unilateral (not symmetric) and may be proximal instead of purely or primarily distal:
-
Small-fiber neuropathies
-
Burning feet syndrome
-
Reflex sympathetic dystrophy
-
Diabetes Mellitus
Also cyclosporine was tried. Cyclosporine may reduce nitric oxide production in vascular smooth-muscle and endothelial cells, resulting in an amelioration of the microvascular abnormalities in erythromelalgia.
Spontaneous remissions may occur. Early-onset disease is relatively unresponsive to treatment and generally is unremitting. Complications appear to be more frequent in patients who clearly have platelet-mediated disease.
